Reducing costs, improving outcomes with AI in a radiology practice
A study published in the Journal of Digital Imaging (2019) [1] looked at whether Artificial Intelligence (AI)-based, computer-aided detection (CAD) software can be used to reduce false positives per image (FPPI) on mammograms as compared to an FDA-approved conventional CAD. The study showed a 69% decrease in FPPI which, the researchers said, could also potentially result in a 17% decrease in radiologist reading time per case. Following this study, CureMetrix, whose AI CAD software was the subject to the study, conducted their own study on how using AI-based mammography solutions could potentially impact a radiology practice’s bottom line. International Hospital speaks to Greg Houlgate, Chief Revenue Officer, CureMetrix about the study and their findings.
International Hospital: CureMetrix has a number of AI CAD products for clinical decision support. Can you tell us which ones were used in the study and briefly give a bit of background about the products?
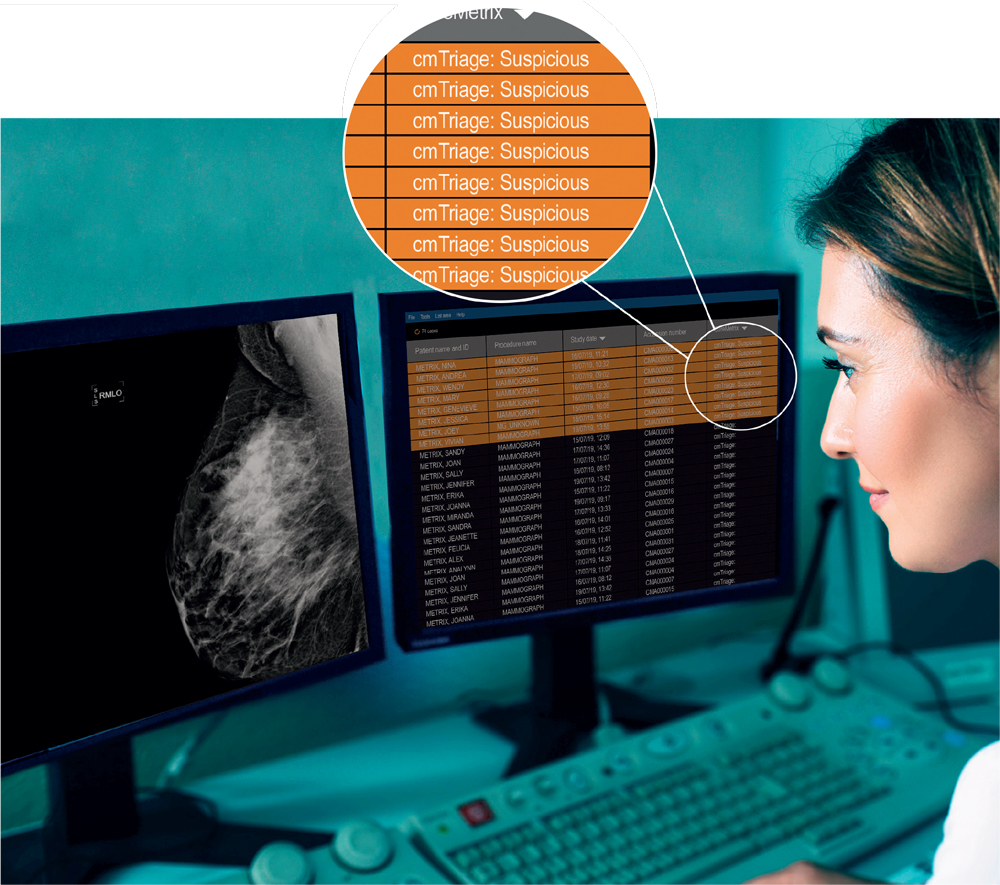
Greg Houlgate: Artificial intelligence (AI), is like a second pair of eyes to support the radiologist. The core AI-based mammography solutions from CureMetrix include cmTriage and cmAssist. cmTriage is the first FDA-cleared AI-based triage solution that helps to triage, sort and prioritize mammography worklists, flagging suspicious cases so that they can be seen at the top of the doctor’s queue.
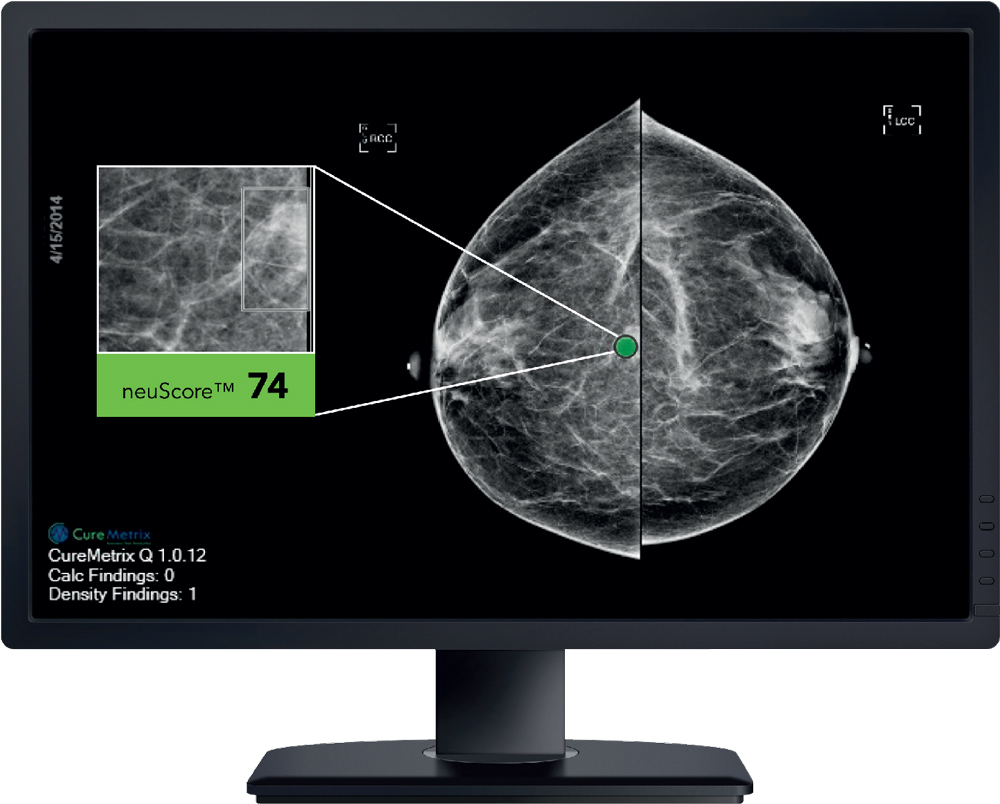
cmAssist is a proprietary, investigational SaaS (Software as a Service) intended to identify, mark and score regions of interest on screening and diagnostic mammograms. cmAssist uses AI to actually mark the mammogram, highlighting identified anomalies. It then gives each mark a unique, data-driven neuScore that illustrates the level of suspiciousness, which informs the radiologist’s decision whether to recall the patient for further screening.
We received our first FDA clearance two years ago, and we are implementing these solutions with key institutions across the globe.
IH: Can you tell us more about your follow-up study?
GH: We have conducted several studies that show how the CureMetrix software can help improve cancer detection, reduce false positives, help radiologists review their cases faster, and provide decision support solutions so that they can improve overall clinical outcomes.
It’s no secret that AI has arrived in radiology and that AI-based CAD is good for patients, but what about AI’s effect on a practice’s revenue? We wanted to explore that. Out of a study with [University of Texas] MD Anderson Cancer Center, we learned that the effect of AI-based CAD was shown to have a sizeable potential impact on the bottom line of a mammography practice – supporting cost savings, improved efficiencies, reduced risk, and expanded marketability of a clinic’s brand to its partners and patients.
IH: From a practical point of view, how would a radiology practice attain the most cost savings by using this AI CAD software?
GH: CureMetrix AI can have a direct impact on the sensitivity, specificity, reading speed, and overall performance of radiologists regardless of their location, volume of mammogram cases, or their years of experience. So from a cost-savings perspective, there are a many ways that AI CAD can help a practice or radiology department realize efficiencies and savings.
First, as shared at the 2020 Radiological Society of North America (RSNA) Annual Meeting, radiologists can read normal cases up to 40 percent faster when aided by CureMetrix solutions. With AI tools, practices can get more done in a day. For example, FDAcleared cmTriage highlights cases most likely to be suspicious and helps radiologists sort their worklists, putting those potentially higher risk cases to the top of their queue.
Next, high false positive rates are common with traditional CAD, which impacts the efficiency of the radiologist and can have a negative impact on the patient experience. With fewer unnecessary markings, a reduction in keystrokes and clicks, and a more focused experience, radiologists can increase their sensitivity, specificity and turnaround time.
Studies have shown that false positives can take between 3-7 seconds to read and disregard. Alone, those may seem like short amounts of time; however, when you consider the number of false positives per image shown with traditional CAD, the number of images per study, and the number of studies per year – those seconds do add up.
Because the AI does the initial review, practices can control relative value units (RVUs) and case distribution for the practice much more efficiently. Overall, a practice can process more mammograms in less time, enabling the doctor to see more patients in a day without increasing physician burn out. All of this can lead to significant savings.
Additionally, AI can help a practice reduce its risk. Key to being successful is reducing your expenses and potential for revenue loss. While your malpractice insurance may cover your practice for a worst-case scenario, CureMetrix AI-based CAD enhances your clinical expertise, it’s a good investment in the financial health of your practice, and even better for your patients’ wellbeing.
IH: In addition to the cost savings opportunities you mentioned, are there revenue generating aspects that AI can bring in supporting a practice?
GH: Promoting a practice organization as being innovative by putting AI in the office is good for overall branding and marketing efforts. From the latest iPhone to solar-powered home energy, consumers have high expectations of technology today and they expect that imaging centres are using state-of-the-art technology to support their clinicians and the care that they deliver to their community. Referring healthcare partners have high expectations, as well.
Solutions like cmTriage and the CureMetrix detection software cmAssist can help a doctor find out if a patient’s mammogram is suspicious before she even leaves the office. The peace of mind this can offer is priceless to the patient – and it is just one example of how using the most cutting-edge AI mammography solutions earns patients’ trust. When patients have a good experience at a practice, they are more likely to return and refer their friends and family members to the facility for radiology services.
IH: From an investment perspective by a radiology practice – what all is required to completely set up this AI CAD system – surely it is not as easy as simply installing new software, or is it?
GH: Implementation of the CureMetrix solutions is very streamlined. Our solutions are cloud based and they integrate with the radiologist’s existing PACS technology, so there is no required hardware installation by the facility. In addition, CureMetrix is integrated with several image management and reporting platforms including Nuance, Ambra and Ikonopedia so installation is just a flip of a switch for practices who are already using those systems.
IH: Are you able to give ballpark costs for this investment?
GH: Investment is minimal, and generally, the cost for solutions is determined based on volume or the number of mammograms that the hospital/centre processes a year. On average, AI-CAD can cost less than a few thousand dollars a month for the entire clinic. In contrast, traditional CAD can cost up to tens of thousands of dollars in hardware and recurring costs for management and support for those older technologies.
IH: Presumably it will depend on the size of the practice, however, with some examples, how long would it take for a practice to see a return on this investment? What sort of cost saving figures are we looking at?
GH: CureMetrix is an investment with very quick returns for the practice. Just by adding up the number of reduced false positives and the increases in reading speed for the radiologists the practice will be able to calculate savings quickly.
In fact, at a hospital such as MD Anderson where over 100,000 mammograms are conducted each year, and based on the study that was conducted showing that CureMetrix AI-CAD had 69% fewer false positive marks, that can add up to a savings of up to 400 hours of labour in just one year.
IH: Besides financial barriers, what other factors do you think may prevent a radiology practice adopting this new AI CAD technology and what do you advise to have them reconsider this investment?
GH: Trust in AI is growing across industries, including the medical field. However, many clinicians are rightfully cautious about adopting new tools and technologies; they want to ensure that they will offer the best outcomes possible for their patients and practices before making them a part of their diagnostic workflow.
Selecting an AI partner that is aligned with the practice’s goals, that delivers quality technology that works across the community’s patient population to deliver cost savings, efficiencies, clinician satisfaction and a better patient experience are all keys to a successful clinical and business outcome. Selecting the wrong vendor or one that is grounded in outdated technology or that is not flexible to support AI, will impede a practice or an institution’s ability to realize savings or capitalize on innovation as it evolves.
What our studies show is that radiologists who work in breast imaging can improve their efficiency, accuracy, overall practice value and job satisfaction by incorporating AI-based mammography solutions into their daily workflow. CureMetrix AI truly puts radiologists in the driver’s seat, empowering them to focus on the most urgent cases, diagnose more quickly and accurately so that they can save more lives – and that has a direct and positive impact on the practice’s bottom line.
For more information, visit: www.CureMetrix.com
Reference
Reduction of False-Positive Markings on Mammograms: a Retrospective Comparison Study Using an Artificial Intelligence-Based CAD. Journal of Digital Imaging. 15 Aug 2019. https://doi.org/10.1007/s10278-018-0168-6