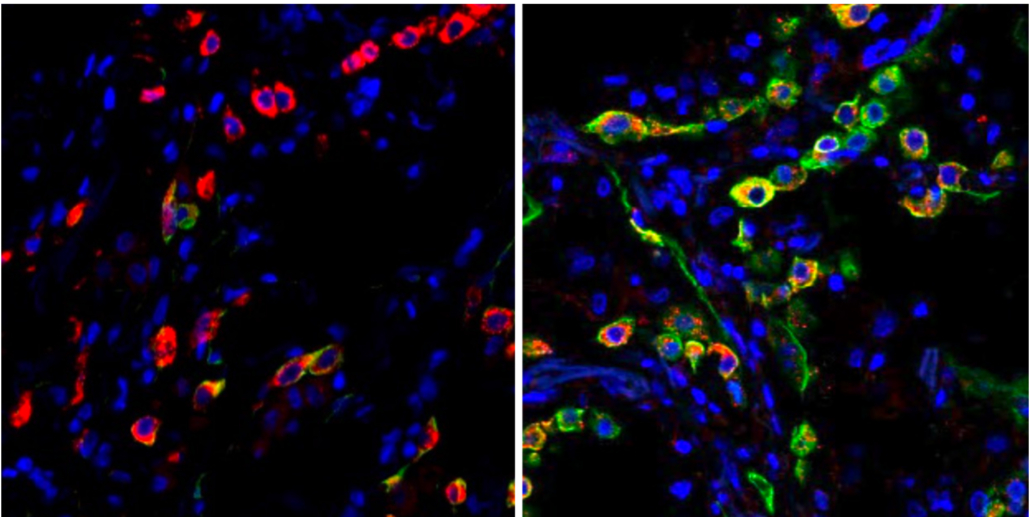
Lung cells in patients with severe COVID become trapped in a state (indicated by the green color) that prevents the cells from repairing damage caused by the infection. The left image shows cells from a healthy lung; the right image shows lung cells from a patient who died from COVID-19. Images: Benjamin Izar / Columbia University Vagelos College of Physicians and Surgeons.
A new study published in Nature [1] draws the most detailed picture yet of SARS-CoV-2 infection in the lung, revealing mechanisms that result in lethal COVID-19, and may explain long-term complications and show how COVID-19 differs from other infectious diseases.
Led by researchers at Columbia University Vagelos College of Physicians and Surgeons and Herbert Irving Comprehensive Cancer Center, the study found that in patients who died of the infection, COVID-19 unleashed a detrimental trifecta of runaway inflammation, direct destruction and impaired regeneration of lung cells involved in gas exchange, and accelerated lung scarring.
Though the study looked at lungs from patients who had died of the disease, it provides solid leads as to why survivors of severe COVID may experience long-term respiratory complications due to lung scarring.
“It’s a devastating disease, but the picture we’re getting of the COVID-19 lung is the first step towards identifying potential targets and therapies that disrupt some of the disease’s vicious circuits. In particular, targeting cells responsible for pulmonary fibrosis early on could possibly prevent or ameliorate long-term complications in survivors of severe COVID-19,” says Benjamin Izar, MD, PhD, assistant professor of medicine, who led a group of more than 40 investigators to complete in several months a series of analyses that usually takes years.
This study and a companion paper [2] led by researchers at Harvard/MIT, to which the Columbia investigators also contributed, were published in the journal Nature on April 29.
Study creates atlas of cells in COVID lung
The new study is unique from other investigations in that it directly examines lung tissue (rather than sputum or bronchial washes) using single-cell molecular profiling that can identify each cell in a tissue sample and record each cell’s activity, resulting in an atlas of cells in COVID lung.
“A normal lung will have many of the same cells we find in COVID, but in different proportions and different activation states,” Izar says. “In order to understand how COVID-19 is different compared to both control lungs and other forms of infectious pneumonias, we needed to look at thousands of cells, one by one.”
Izar’s team examined the lungs of 19 individuals who died of COVID-19 and underwent rapid autopsy (within hours of death) – during which lung and other tissues were collected and immediately frozen – and the lungs of non-COVID-19 patients. In collaboration with investigators at Cornell University, the researchers also compared their findings to lungs of patients with other respiratory illnesses.
Drugs targeting IL-1ß may reduce inflammation
Compared to normal lungs, lungs from the COVID patients were filled with immune cells called macrophages, the study found.
Typically during an infection, these cells chew up pathogens but also regulate the intensity of inflammation, which also helps in the fight.
“In COVID-19, we see expansion and uncontrolled activation of macrophages, including alveolar macrophages and monocyte-derived macrophages,” Izar says. “They are completely out of balance and allow inflammation to ramp up unchecked. This results in a vicious cycle where more immune cells come in causing even more inflammation, which ultimately damages the lung tissue.”
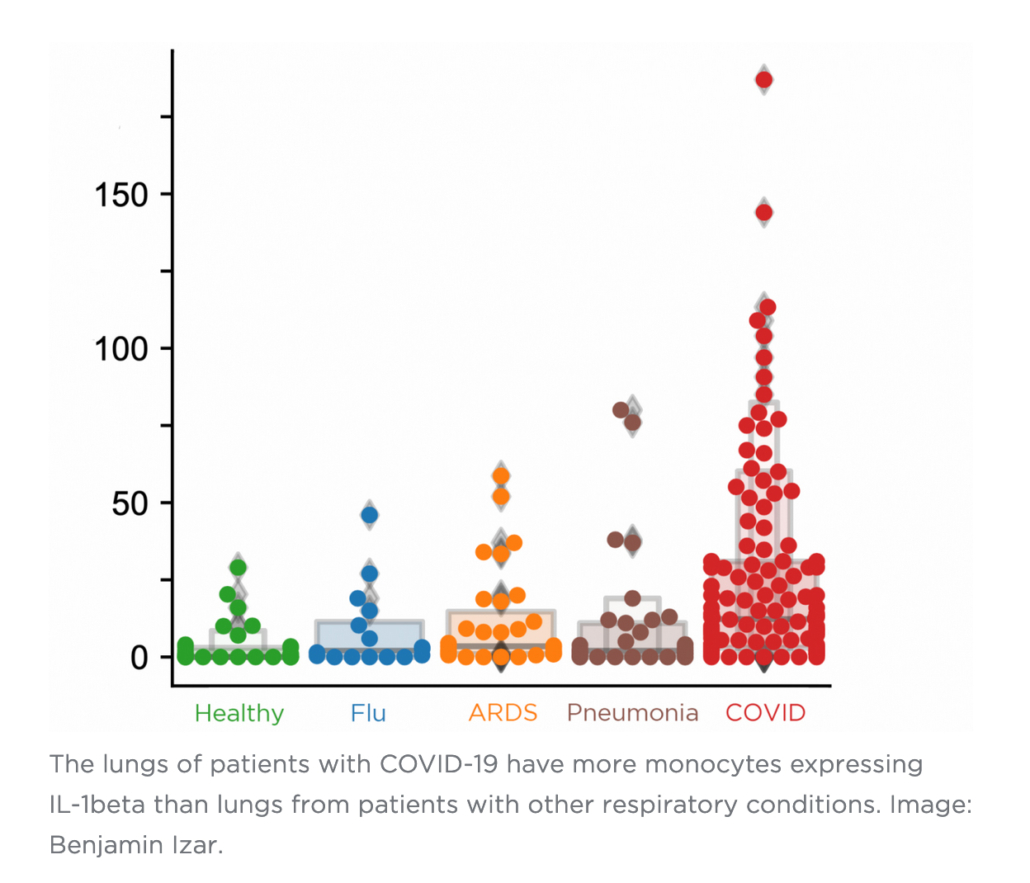
One inflammatory cytokine in particular, IL-1ß, is produced at a high rate by these macrophages.
“Unlike other cytokines such as IL-6, which appears to be universally prevalent in various pneumonias, IL-1ß production in macrophages is more pronounced in COVID-19 compared to other viral or bacterial lung infections,” Izar says. “That’s important because drugs exist that tamp down the effects of IL-1ß.”
Some of these drugs are already being tested in clinical trials of COVID patients.
Severe COVID also prevents lung repair
In a typical infection, a virus damages lung cells, the immune system clears the pathogen and the debris, and the lung regenerates.
But in COVID, the new study found that not only does SARS-CoV-2 virus destroy alveolar epithelial cells important for gas exchange, the ensuing inflammation also impairs the ability of the remaining cells to regenerate the damaged lung.
Though the lung still contains cells that can do the repairs, inflammation permanently traps these cells in an intermediate cell state and leaves them unable to complete the last steps of differentiation needed for replacement of mature lung epithelium.
“Among others, IL-1ß appears to be a culprit in inducing and maintaining this intermediate cell state,” says Izar, “thereby linking inflammation and impaired lung regeneration in COVID-19. This suggests that in addition to reducing inflammation, targeting IL-1ß may help take the brakes off cells required for lung repair.”
Preventing accelerated fibrosis
The researchers also found a large number of specific fibroblast cells, called pathological fibroblasts, that create rapid scarring in COVID-19 lungs. When the fibroblast cells fill the lung with scar tissue, a process called fibrosis, the lung has less space for cells involved in gas exchange and is permanently damaged.
Given the importance of pathological fibroblasts in the disease, Izar’s team closely analysed the cells to uncover potential drug targets. An algorithm called VIPER, developed previously by Andrea Califano, Dr, chair of systems biology at Columbia University Vagelos College of Physicians and Surgeons, identified several molecules in the cells that play an important role and could be targeted by existing drugs.
“This analysis predicted that inhibition of STAT signalling could alleviate some of the deleterious effects caused by pathological fibroblasts,” Izar says.
“Our hope is that by sharing this analysis and massive data resource, other researchers and drug companies can begin to test and expand on these ideas and find treatments to not only treat critically ill patients, but also reduce complications in people who survive severe COVID-19.”
References
[1] A molecular single-cell lung atlas of lethal COVID-19. Nature (2021).
https://doi.org/10.1038/s41586-021-03569-1
[2] COVID-19 tissue atlases reveal SARS-CoV-2 pathology and cellular targets. Nature (2021).
https://doi.org/10.1038/s41586-021-03570-8

First global study of pandemic’s impact on childhood cancer care reveals worldwide effects
, /in Featured Articles /by panglobalThe COVID-19 pandemic has had major impacts on childhood cancer care worldwide, according to a survey of more than 300 clinicians from 200 hospitals worldwide published in The Lancet Child & Adolescent Health journal.
Breaking down barriers to sourcing life-saving medications
, /in Featured Articles /by panglobalInternational Hospital speaks to Sjaak Vink, CEO and Founder of TheSocialMedwork about the organisation and how it is helping patients source medications unavailable in their country of residence.
Reinforcing sharps safety beyond the hospital
, /in Featured Articles /by panglobalBy George I’ons, Head of Product Strategy and Insights, Owen Mumford Pharmaceutical Services
Trauma and emergency surgeons positively impact patient satisfaction
, /in Featured Articles /by panglobalTrauma patients and patients who need emergency surgery have little to no opportunity to get acquainted with the surgeon and team that will perform their operation. However, a large study has found that effective and meaningful physician communication is a more important contributor to the overall satisfaction of trauma patients and those having emergency surgery […]
New Cell Atlas of COVID lungs reveals why SARS-CoV-2 is different and deadly
, /in Corona News, E-News /by panglobalLung cells in patients with severe COVID become trapped in a state (indicated by the green color) that prevents the cells from repairing damage caused by the infection. The left image shows cells from a healthy lung; the right image shows lung cells from a patient who died from COVID-19. Images: Benjamin Izar / Columbia University Vagelos College of Physicians and Surgeons.
A new study published in Nature [1] draws the most detailed picture yet of SARS-CoV-2 infection in the lung, revealing mechanisms that result in lethal COVID-19, and may explain long-term complications and show how COVID-19 differs from other infectious diseases.
Led by researchers at Columbia University Vagelos College of Physicians and Surgeons and Herbert Irving Comprehensive Cancer Center, the study found that in patients who died of the infection, COVID-19 unleashed a detrimental trifecta of runaway inflammation, direct destruction and impaired regeneration of lung cells involved in gas exchange, and accelerated lung scarring.
Though the study looked at lungs from patients who had died of the disease, it provides solid leads as to why survivors of severe COVID may experience long-term respiratory complications due to lung scarring.
“It’s a devastating disease, but the picture we’re getting of the COVID-19 lung is the first step towards identifying potential targets and therapies that disrupt some of the disease’s vicious circuits. In particular, targeting cells responsible for pulmonary fibrosis early on could possibly prevent or ameliorate long-term complications in survivors of severe COVID-19,” says Benjamin Izar, MD, PhD, assistant professor of medicine, who led a group of more than 40 investigators to complete in several months a series of analyses that usually takes years.
This study and a companion paper [2] led by researchers at Harvard/MIT, to which the Columbia investigators also contributed, were published in the journal Nature on April 29.
Study creates atlas of cells in COVID lung
The new study is unique from other investigations in that it directly examines lung tissue (rather than sputum or bronchial washes) using single-cell molecular profiling that can identify each cell in a tissue sample and record each cell’s activity, resulting in an atlas of cells in COVID lung.
“A normal lung will have many of the same cells we find in COVID, but in different proportions and different activation states,” Izar says. “In order to understand how COVID-19 is different compared to both control lungs and other forms of infectious pneumonias, we needed to look at thousands of cells, one by one.”
Izar’s team examined the lungs of 19 individuals who died of COVID-19 and underwent rapid autopsy (within hours of death) – during which lung and other tissues were collected and immediately frozen – and the lungs of non-COVID-19 patients. In collaboration with investigators at Cornell University, the researchers also compared their findings to lungs of patients with other respiratory illnesses.
Drugs targeting IL-1ß may reduce inflammation
Compared to normal lungs, lungs from the COVID patients were filled with immune cells called macrophages, the study found.
Typically during an infection, these cells chew up pathogens but also regulate the intensity of inflammation, which also helps in the fight.
“In COVID-19, we see expansion and uncontrolled activation of macrophages, including alveolar macrophages and monocyte-derived macrophages,” Izar says. “They are completely out of balance and allow inflammation to ramp up unchecked. This results in a vicious cycle where more immune cells come in causing even more inflammation, which ultimately damages the lung tissue.”
One inflammatory cytokine in particular, IL-1ß, is produced at a high rate by these macrophages.
“Unlike other cytokines such as IL-6, which appears to be universally prevalent in various pneumonias, IL-1ß production in macrophages is more pronounced in COVID-19 compared to other viral or bacterial lung infections,” Izar says. “That’s important because drugs exist that tamp down the effects of IL-1ß.”
Some of these drugs are already being tested in clinical trials of COVID patients.
Severe COVID also prevents lung repair
In a typical infection, a virus damages lung cells, the immune system clears the pathogen and the debris, and the lung regenerates.
But in COVID, the new study found that not only does SARS-CoV-2 virus destroy alveolar epithelial cells important for gas exchange, the ensuing inflammation also impairs the ability of the remaining cells to regenerate the damaged lung.
Though the lung still contains cells that can do the repairs, inflammation permanently traps these cells in an intermediate cell state and leaves them unable to complete the last steps of differentiation needed for replacement of mature lung epithelium.
“Among others, IL-1ß appears to be a culprit in inducing and maintaining this intermediate cell state,” says Izar, “thereby linking inflammation and impaired lung regeneration in COVID-19. This suggests that in addition to reducing inflammation, targeting IL-1ß may help take the brakes off cells required for lung repair.”
Preventing accelerated fibrosis
The researchers also found a large number of specific fibroblast cells, called pathological fibroblasts, that create rapid scarring in COVID-19 lungs. When the fibroblast cells fill the lung with scar tissue, a process called fibrosis, the lung has less space for cells involved in gas exchange and is permanently damaged.
Given the importance of pathological fibroblasts in the disease, Izar’s team closely analysed the cells to uncover potential drug targets. An algorithm called VIPER, developed previously by Andrea Califano, Dr, chair of systems biology at Columbia University Vagelos College of Physicians and Surgeons, identified several molecules in the cells that play an important role and could be targeted by existing drugs.
“This analysis predicted that inhibition of STAT signalling could alleviate some of the deleterious effects caused by pathological fibroblasts,” Izar says.
“Our hope is that by sharing this analysis and massive data resource, other researchers and drug companies can begin to test and expand on these ideas and find treatments to not only treat critically ill patients, but also reduce complications in people who survive severe COVID-19.”
References
[1] A molecular single-cell lung atlas of lethal COVID-19. Nature (2021).
https://doi.org/10.1038/s41586-021-03569-1
[2] COVID-19 tissue atlases reveal SARS-CoV-2 pathology and cellular targets. Nature (2021).
https://doi.org/10.1038/s41586-021-03570-8
UPGRADE YOUR OPERATING ROOM
, /in Advertenties /by 3wmediaWhole Blood Glucose Reference Analyzer
, /in Advertenties /by panglobalNew! – Introducing 3D Ultrasound for Breast Imaging, Powered by UltraFast Technology
, /in Advertenties /by HOLOGIC NVCALL FOR ABSTRACTS
, /in Advertenties /by panglobalPSA Systems safeguard oxygen supplies during crisis
, /in Product News /by panglobalThe coronavirus pandemic has revealed flaws in the global supply chain for oxygen that can put virus patients’ lives at risk. David Cheeseman, Chief Engineer of Oxair Gas Systems, a leading global supplier of on-site gas generating equipment, explains how the latest technology can replace outsourcing conventional oxygen tanks.
The Covid-19 pandemic has resulted in dwindling oxygen supplies as demand soared during the crisis, with deadly consequences for patients, particularly in countries suffering high infection rates. Generating a constant flow of oxygen on site helps hospitals save lives by becoming less reliant on outsourcing conventional canisters.
Severe shortages of this life-saving gas were reported from all corners of the world during the pandemic, raising concerns that fault lines have been exposed in the supply chain with hospitals being forced to ration oxygen to avoid the risk of running out.
Off-the-shelf automated solution
There is an off-the-shelf automated solution to avoid potential shortages in the form of Oxygen Pressure Swing Adsorption (PSA) systems, robust technology which has been designed to deliver consistent, high purity oxygen on tap to hospitals and medical facilities even in the remotest locations around the world.
Medical facilities are often forced to rely on outsourcing oxygen, with failing supply lines posing a potential catastrophe for hospitals, not to mention the added stress on frontline staff associated with the storage, handling and removal of traditional oxygen cylinders.
PSA medical oxygen offers better patient care with a permanent flow of high-quality oxygen to suit the needs of the hospital – and the equipment is capable of piping oxygen around every department as needed. In cases where the hospital does not have a central piping system, suppliers like Oxair will install an onsite cylinder filling system. It’s a highly cost-effective and hygienic alternative to the inconvenience and uncertainty of outsourcing canisters.
Constant oxygen
This automated system delivers constant oxygen of 94-95 percent purity through PSA filtration, a unique process that separates oxygen from compressed air. The gas is then conditioned and filtered before being stored in a buffer tank to be used directly by the hospital on demand.
It’s not just in the middle of a global pandemic when outsourcing conventional canisters can hit a bottleneck. Ensuring a reliable supply to hospitals in remote or troubled locations proves a constant challenge when faced with poor infrastructure, limited resources and haphazard road conditions.
An ideal example, Heal Africa hospital in The Democratic Republic of the Congo (DRC), had been relying on tanker deliveries of oxygen from a neighbouring state, but staff found that patients were being left at risk due to faulty equipment which, upon testing, was discovered to be supplying just 60 percent oxygen purity compared with the standard 93 percent needed for medical grade applications.
Supply difficulties
It was decided that a new oxygen system was vital and the hospital was able to overcome its supply difficulties by having an Oxair OA450 system installed, piping oxygen around the hospital to every department as needed, providing a cost-effective and hygienic alternative to the inconvenience of ordering in traditional carbon steel cylinders which are also prone to corrosion.
Meanwhile, medical facilities on the subcontinent have not only seen the life-saving benefits of turning to automation but cost savings too. The Sunrise Hospital in Hyderabad, India, installed a PSA system to supply its oxygen – saving the hospital almost a thousand pounds a month by reducing its dependence on cylinders.
The multi-specialist facility was going through cylinders at a costly rate of up to 16 a day. Now Sunrise’s owner is happy because the hospital is saving money which can be redirected to improving other services, while the staff are happy because they have more time to care for patients.
By embracing an automated process, Sunrise is following in the footsteps of many other hospitals in the Indian medical sector that have realised the benefits of having their own source of oxygen, helping to eliminate possible future interruptions.
To improve the flow of oxygen, suppliers should be ready to step up and do whatever is necessary to help healthcare services during the current coronavirus crisis – and beyond – by providing life-saving oxygen equipment wherever it is needed.
Plug-and-play
PSA systems that are ‘plug-and-play’ means that they are literally ready to start working as soon as they are delivered and plugged in – with voltage adapted to the country of delivery. Wherever they may be located, hospitals can rely on technology which is tried and tested over many years, coupled with almost instant access to vital oxygen supplies.