Obtaining more information: Uncontrasted Computed Tomography or ultrasound?
This article compares uncontrasted Computed Tomography (CT) with ultrasound examinations over a period of a year (from May 2011 to May 2012) with data obtained from a private practice PACS database. All the uncontrasted studies which had been performed were considered for the study: 339 patients were included in the research done for this investigation. The uncontrasted CT request forms, images and radiologist reports were audited by the author. Although the answer seems obvious, the outcome of the study revealed much more than initially anticipated.
by Dr Jaco Parsons
For a radiologist working in a private practice, it is of the utmost importance to give the referring clinician detailed information about the patient. It is also essential to use the right tools to make a correct and speedy diagnosis for the sake of the patient. Bearing this basic principle in mind, the question arose whether uncontrasted Computed Tomography gives better delineation of pathology than ultrasound.
In the South African context, medical aid is mainly private and thus very costly. Therefore, when the radiologist has to determine the type of investigation, it is often easier to take the route of least resistance and opt for the cheaper choice. Ethically, this may be doing the patient an injustice and may cause a delay in reaching the right diagnosis.
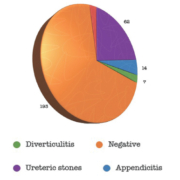
Study sample of CT
The data used comprised a set of 339 patients which were then entered and analysed. No distinction was made between male and female patients; the mean age was 48 years. In total, 193 (56.9%) studies were negative for the specific request. Twenty-four different types of requests were registered; the main request categories included 173 (51%) for ureteric stones, 84 (24.7%) abdominal pain, 13 (3.8%) appendicitis and 9 (2.6%) diverticulitis. Based on the main requests, it became clear that the following requests were negative: 112 (64.7%) for ureteric stones; 39 (46.4%) for abdominal pain; 13 (46.1%) for appendicitis; and 5 (55.5%) for diverticulitis.
In total, 62 (18%) studies had ureteric stones, 48 (14%) renal stones, 23 (6.7%) diverticulae, 22 (6.5%) renal cysts, 15 (4.4%) lumbo-sacral spondylosis, 15 (4.4%) hernias, 14 (4.1%) appendicitis and 13 (3.8%) gall stones. Moreover, there were 46 different