Making emergency department handover Lean
Inter-shift handover in the emergency department (ED) has long been identified as a high risk undertaking when it comes to patient safety. At the Graduate Entry Medical School, University of Limerick, the Lean process has been instrumental in helping to find solutions to current challenges in the emergency department.
by Dr Rosa McNamara and Dr Fergal Cummins
Patient handover is the term used to describe the act of transferring care from one healthcare professional to another. The terms ‘patient handoff’, ‘sign-out’ and ‘transitions of care’ are also used to describe this process. The act of handover has been identified as a risk in terms of patient safety, and has been described as a point where safety often fails first [1]. Faulty handoffs have been specifically implicated in 24% of malpractice claims in the Emergency Department [2].
Poor handover is associated with a number of adverse effects such as having to re-examine or re-interview the patient [4] inaccurate clinical assessment, delayed diagnosis, delayed investigation, medication errors, inconsistent or incorrect results translation, duplication of results, increased length of stay in hospital, increased in-hospital complications, and decreased patient satisfaction [3].
In a large prospective study, 914 patients were observed during 60 handovers in three metropolitan EDs [4]. They found that information was lacking in 15.4% of handovers, such as information on management, investigations or disposition. In these cases, 56.9% resulted in an adverse event for the doctor and 30.3% for the patient. Adverse events for the doctor included duplication of work, for example, re-interviewing or re-examination of the patient.
Although scripting or verbal standardisation has been recommended [5], a satisfactory and reliable tool to improve quality of ED handover remains elusive [6,7].
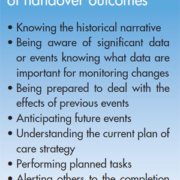
Recently, the American College of Emergency Physicians published a document detailing the current evidence regarding ED handoff, providing, a list of suggested handover quality measures, amongst other recommendations [8].
The Department of Emergency Medicine at the University Hospital, Limerick, sees approximately 60 000 patients per year. By applying these standards, it became clear that existing handover processes were inefficient and potentially posed a threat to patient safety. Formal documentation of handover on written notes was low. Only 6% of notes − on audit − met the standards suggested by the American College of Emergency Physicians.
During the auditing of the handover process, it became very clear that there was duplication of history taking and patient examination. After action group meetings within the ED between senior and junior medical staff, an initial decision was made to introduce a formal board round, and new policies were brought in to ensure handover was recorded using the electronic patient tracker programme (MAXIMS