Interventional cardiology: from keyhole to pinhole
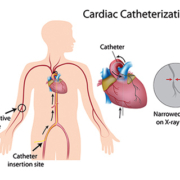
Interventional cardiology, like minimally invasive surgery, has for decades been driven by miniaturization. New lightweight, biocompatible and sometimes self-expanding materials (for catheters and stents), alongside sophisticated digital imaging algorithms, have been the key technology enablers. These, in turn, have reduced vascular complications and hemostasis as well as the use of contrast agents
The emergence of transradial access
One recent development is transradial access, where a catheter is introduced through the radial rather than femoral artery. Making this feasible has been the arrival of automated contrast injectors which permit improvements in angiographic image resolution.
Typically, smaller catheters in use today are 5 Fr. Sheathless catheters promise to reduce the miniaturization envelope even further, since the catheter sheath typically adds 1-2 Fr in diameter. In such circumstances, some foresee a future with what are effectively equivalent to 3 Fr interventions based on a 4 or 5 Fr sheathless catheter.
Cardiologists divided over smaller catheters
However, there is still doubt about the impact of smaller catheters on procedural efficiency and outcomes. In turn, this dovetails into a longer-running debate about the utility of radial access (one of the drivers of demand for smaller catheters) versus the femoral route.
Interventional cardiologists seem divided into two camps on the issue.
The first consists of those who believe 6 Fr (considered