Beckman Coulter assists expansion of national network of HIV testing in Uganda
By Samuel Boova, Director Alliance Development, High Burden HIV Global Markets, Beckman Coulter Life Sciences
Despite significant progress in its prevention and treatment, human immunodeficiency virus (HIV) remains a serious public health threat across the globe. The United Nations programme UNAIDS has led the global effort to address the HIV/AIDS crisis and has set out its 90-90-90 target: 90 percent of all people living with HIV (PLHIV) will know their HIV status, 90 percent of those diagnosed will receive antiretroviral therapy (ART), and 90 percent of those receiving ART will have viral suppression and not infect others [1].
Unfortunately, even the first of the UNAIDS 90-90-90 goals has been challenging, and there remains a large percentage of the 37 million PLHIV who are unaware of their status. The first UNAIDS goal of 90 percent of all PLHIV will know their HIV status is estimated to be about 80 percent globally, and even lower in areas with higher disease burden (e.g., 40 percent in some Sub Saharan Africa countries) [2].
Making the situation more urgent is that PLHIV may have Advanced HIV Disease (AIDS) and be at higher risk for opportunistic infections (OI), including tuberculosis, cryptococcal meningitis, and respiratory infection, which themselves can be fatal [3].
There are several challenges inherent in reaching the testing goal in any location – the logistics, deployment, and cost of widespread laboratory testing on the provider side, and access and willingness on the patient side, among others. Challenging, too, is that two-thirds of the world’s PLHIV are in Sub-Saharan Africa, where the remoteness of both residents and clinics, harsh climates, and lack of resources can add to the difficulty in implementing widespread diagnostic programmes [2].
The COVID-19 pandemic has further disrupted routine testing and supply chains for HIV. Beckman Coulter Life Sciences have partnered with organizations both here in the U.S. and in Africa, to address some of these issues. In particular, we’ve helped deploy instruments to expand testing for people who may not know their status, especially in remote areas.
Testing for HIV generally falls into two categories: viral load analysis and immune status, or CD4, testing. Viral load testing is used to track the amount of virus a person has and determine whether ART is successful. It’s become the recommended strategy for monitoring a patient’s disease status over time, and some countries have begun to use only this method.
However, CD4 testing remains an important tool, since it provides insight into the state of a person’s immune system and their risk for OI. In CD4 testing, the number of CD4 cells are measured — CD4 is a protein on the surface of white blood cells known as T helper cells, which scout out and destroy pathogens. Low CD4 counts may mean that ART is not working or that the person has more advanced HIV. Patients with very low CD4 counts are likely to need specific drugs to prevent specific OIs, in addition to their ART. The World Health Organization’s Advanced HIV Disease challenge has brought more emphasis back to CD4 testing, since mortality rates remain a concern and OIs remain a risk factor [3]. CD4 testing is done via flow cytometry, which uses antibodies that recognize specific markers on the surface of or inside immune cells – the markers’ pattern can identify the cell type.
Some countries in Africa, namely Uganda, Lesotho, Botswana, South Africa and Namibia, all run successful CD4 programmes. But for many areas, procuring the flow cytometers, along with the required reagents, remains a challenge. Much of this is due to the financial resources required to implement standardized testing through a national laboratory system. Since 2015, Beckman Coulter Life Sciences has worked with the Ugandan Ministry of Health through the National Public Health Laboratory Service. Having already implemented a successful CD4 programme, Uganda invited us to tour and evaluate the country’s laboratory system. We ultimately instituted a partnership to enhance certain aspects of their system, namely, to improve costs and turnaround times, and to boost demand for testing.
As part of this initiative, we’ve been invited to provide our high-throughput AQUIOS CL flow cytometer to process higher demand for patient testing in Uganda. The AQUIOS CL is the only automated high-throughput system to be WHOprequalified for use in resource-limited settings. Its key benefits are automated loading and sample preparation, along with its reagent management system. The operator does not need previous flow cytometry experience, so it’s useful for labs that may not have highly trained staff. Finally, the operator doesn’t come into contact with blood samples, which makes it especially safe to run; because of this, it meets the U.S. Centers for Disease Control and Prevention’s biosafety criteria for protecting operators against infectious agents, including COVID-19 [4,5].
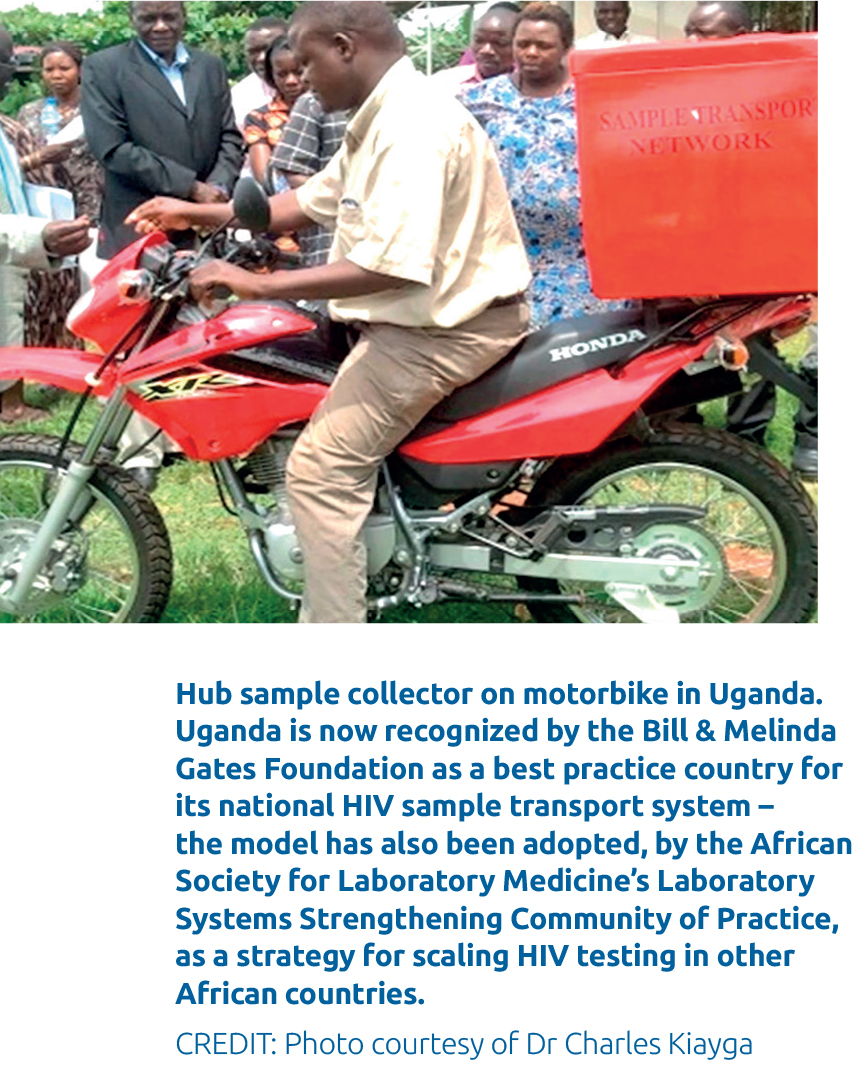
The Uganda ministry of health and national laboratory services have both centralized testing for high-throughput patient testing and point of care for more remote areas. Uganda is now recognized by the Bill & Melinda Gates Foundation as a best practice country for its national sample transport system – the model has also been adopted, by the African Society for Laboratory Medicine’s Laboratory Systems Strengthening Community of Practice (LabCoP), as a strategy for scaling HIV testing in other African countries. AQUIOS can help meet the increased demand for high-throughput centralized test facilities in countries that have adopted LabCoP best practices for national sample transport. As part of our ongoing commitment for Global Health we have collaborated with several other organizations, including the ASCP Global Health, AMPATH Laboratories at Moi Teaching and Referral Hospital (MTRH), and ICAP-CQUIN at Columbia University Mailman School of Public Health. Our mission for the CARES Initiative extends to additional areas that could benefit from laboratory system strengthening, such as cancer diagnosis – and we’ve partnered with relevant organizations (e.g., Burkitt’s Lymphoma Fund for AFRICA). With them, we’re working to improve diagnostics access and workflow in low- and middle-income countries for blood cancers (leukaemia and non-Hodgkin’s lymphoma), especially in paediatric patients.
Ending public health crises requires large scale health and development efforts, multi-sectoral partnerships, and evidence-based action. We invite all global organizations, life sciences and otherwise, to assist where they can in helping lay the foundation for a healthier and more equitable world.
References:
- UNAIDS.org, https://www.unaids.org/en/resources/factsheet (accessed 27 October 2020).
- Avert.org, https://www.avert.org/global-hiv-and-aidsstatistics (accessed 27 October 2020).
- WHO, (2017), Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy, Geneva: World Health Organization.
- US Centers for Disease Control and Prevention (CDC): “Interim Laboratory Biosafety Guidelines for Handling and Processing Specimens Associated with Coronavirus Disease 2019 (COVID-19)” https://www.cdc.gov/ coronavirus/2019-ncov/lab/lab-biosafety-guidelines.html (accessed 2 April 2020).
- European Centre for Disease Prevention and Control (ECDC): “Laboratory support for COVID-19 in the EU/ EEA”. https://www.ecdc.europa.eu/en/novel-coronavirus/ laboratory-support (accessed 2 April 2020).