Retinal stem cells discovered by scientists offer hope for regenerative eye therapies
Scientists have discovered two populations of stem cells in the retina with strong regenerative properties, according to a new study published in Science Translational Medicine. The research team identified human neural retinal stem-like cells (hNRSCs) that can differentiate into light-sensing cells, offering a potential source of stem cells for regenerative eye therapies.
Retinal damage is one of the leading causes of blindness worldwide, but current treatments can only slow the degeneration of neural retina (NR) cells, without actually regenerating lost cells. This breakthrough finding could transform how we treat retinal diseases in the future.
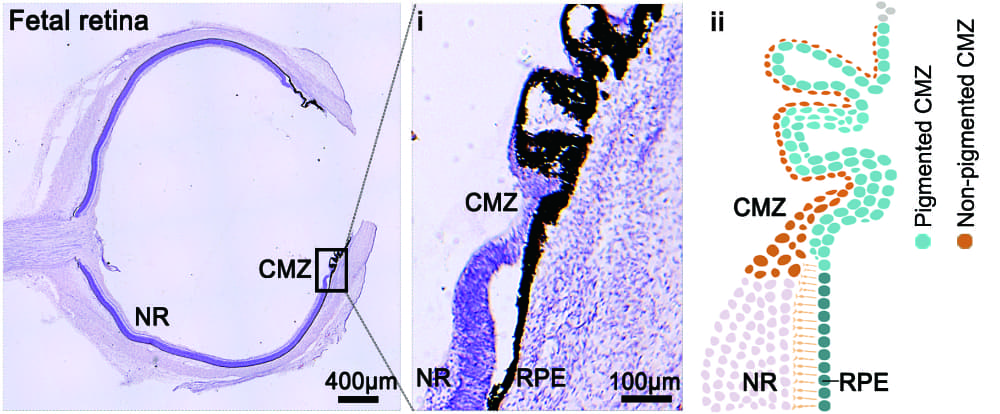
H&E staining of an 18-week human fetal retina, showing the spatial distribution and differentiation potential of human retinal stem cells in the ciliary marginal zone. © Jianzhong Su, State Key Laboratory of Eye Health, Eye Hospital, Wenzhou Medical University
Two distinct stem cell populations identified
Researchers from Wenzhou Medical University and collaborating institutions used cutting-edge single-cell analysis techniques to investigate human foetal retinas and laboratory-grown retinal organoids. They discovered two distinct populations of stem-like cells in the ciliary marginal zone (CMZ) – a specialized region at the edge of the retina.
“We identified two stem cell subpopulations in the human foetal retina: hNRSCs and RPE stem-like cells, which give rise to neural retina and retinal pigment epithelium lineages,” the authors explain in their paper. “hNRSCs differed from traditional retinal progenitor cells, exhibiting enhanced self-renewal capabilities.”
These stem cells were located in separate anatomical locations within the CMZ. The hNRSCs were found in the peripheral retina within the non-pigmented CMZ, while RPE stem-like cells were found adjacent to the hNRSC cluster and connected to the retinal pigment epithelium layer.
The research team confirmed that hNRSCs could form clonal spheres in laboratory culture and differentiate into various retinal cell types, including retinal progenitor cells, retinal ganglion cells, photoreceptors, horizontal cells, amacrine cells, bipolar cells, and Müller glial cells.
Lab-grown organoids mirror foetal retina
A significant aspect of the study involves retinal organoids – three-dimensional structures grown from stem cells that mimic the developing retina. The research team found that approximately 80% of these organoids developed CMZ-like structures containing stem cells with properties remarkably similar to those found in foetal retinas.
To understand the repair potential of these stem cells, the researchers surgically removed neural retina regions from the organoids while preserving the CMZ. Through time-lapse imaging, they observed the progressive repair of the excised portions, with new retinal cells developing from the preserved CMZ.
“We found that the hNRSCs in the CMZ of retinal organoids closely resemble those found in the foetal retina and elucidated their roles in mediating retinal repair,” the authors noted in their discussion.
Molecular analysis revealed that a transcription factor called MECOM plays a crucial role in this regenerative process. When the researchers knocked out MECOM in hNRSCs, retinal repair was significantly impaired, demonstrating its importance in the regenerative pathway.
Transplantation improves vision in mice
The most compelling evidence for the therapeutic potential of these stem cells came from transplantation experiments. The team isolated hNRSCs from retinal organoids and transplanted them into the subretinal spaces of mice with retinitis pigmentosa, a degenerative eye disease.
Twelve weeks after transplantation, the researchers observed that the transplanted cells had differentiated into various retinal cell types and integrated into the host retina. More importantly, these mice showed improved visual function compared to control groups, as measured by electroretinography and visual acuity tests.
“In comparison with the control groups, the hNRSC-transplanted groups exhibited improvement at 4, 8, 12, 16, and 20 weeks post-transplantation,” the researchers report.
Safety assessments showed no tumour formation in eyes transplanted with hNRSCs up to 80 days post-transplantation, whereas tumours developed in 8 of 10 cases when embryonic stem cells were transplanted, highlighting the safety advantage of using hNRSCs.
Future therapeutic potential
The authors believe these findings have significant implications for treating retinal degenerative diseases.
“In conclusion, we have identified a unique population of hNRSCs located within the CMZs of both foetal retinas and retinal organoids. These cells exhibit capabilities for self-renewal and differentiation into all types of retinal cells,” they write. “The significance of this research not only deepens our understanding of retinal biology but also holds immense potential for advancing therapeutic interventions in retinal degenerative diseases.”
While the research shows promising results in mice, further studies will be needed to determine if similar benefits can be achieved in humans. The researchers point out that long-term safety assessments in mice and primates will be necessary, along with better understanding of the mechanisms behind hNRSC-mediated retinal repair.
Nevertheless, this discovery represents a significant advance in the field of regenerative medicine for eye diseases, potentially offering a new approach to restore vision in patients with retinal damage.
Reference:
Liu, H., Ma, Y., Gao, N., et. al. (2025). Identification and characterization of human retinal stem cells capable of retinal regeneration. Science Translational Medicine, 17(788), adp6864. https://doi.org/10.1126/scitranslmed.adp6864

