Reimagine OSA treatment: Moving beyond CPAP for lifelong health benefits
Sleep works as the body’s natural reset – a time for the mind to recharge and the body to restore itself. Yet, for millions suffering from obstructive sleep apnea (OSA), restful sleep remains elusive. Instead of renewal, they endure interrupted breathing and fragmented rest, leading to an increased risk of serious health issues.
By R. Kirk Huntsman,
Chairman and CEO, Co-Founder at Vivos Therapeutics
OSA affects nearly every aspect of health and well-being, making effective, sustainable treatment critical. Recent advancements in non-invasive solutions targeting the root causes of OSA offer a promising shift in how this condition is managed. For healthcare leaders, addressing this unmet need presents an opportunity to improve patient outcomes and explore innovative therapies that redefine treatment standards.
Why OSA demands attention
The consequences of OSA extend far beyond poor sleep, contributing to chronic fatigue, reduced productivity, and increased risks of cardiovascular disease, hypertension, stroke, and even certain cancers.
In the United States, OSA affects an estimated 90 million adults and children, yet up to 90% of cases remain undiagnosed. Many individuals mistakenly attribute symptoms such as snoring, fatigue, and daytime drowsiness to age, stress, or lifestyle factors. This delayed recognition exacerbates the risks and burdens associated with the condition.
OSA in women is often underdiagnosed due to its atypical presentation. While men frequently exhibit loud snoring and gasping for air, women may experience subtler symptoms, such as insomnia, depression, or chronic fatigue, particularly after menopause. This oversight highlights the need for increased awareness and a more comprehensive approach to identifying at-risk populations.
The diagnostic challenges of OSA
A significant barrier to effective management of OSA lies in the complexities of its diagnosis. Despite its prevalence, the condition often goes undetected due to its silent and misunderstood nature. Patients’ misperception delays early intervention, leaving the condition untreated until it progresses to more severe stages, where the risks of cardiovascular disease, diabetes, and cognitive decline significantly increase.
This lack of awareness and understanding hinders timely treatment, creating a ripple effect on patients’ health and healthcare systems. Increasing education for both healthcare providers and the public is critical to closing this gap. Early diagnosis, facilitated by advanced screening tools and awareness campaigns.
The cost of untreated OSA
Beyond personal health, untreated OSA poses broader social and economic challenges. Fatigue-related workplace errors and motor vehicle accidents are common consequences, underscoring the societal impact of this condition.
In children, untreated OSA may manifest as attention deficits, hyperactivity or behavioral issues, bedwetting, lower IQ, stunted growth, chronic allergies or more, and is often undiagnosed or mistaken for other conditions. Early diagnosis and intervention can have profound implications for their development and long-term quality of life.
Current treatment limitations
Continuous positive airway pressure (CPAP) therapy has long been the gold standard for OSA treatment. While effective, CPAP requires patients to wear a mask connected to a machine, which many find uncomfortable, noisy, and inconvenient. Studies indicate that nearly a third of CPAP users discontinue use over time due to these challenges, while other unpublished real-world data suggests as many as 88% eventually abandon regular CPAP usage. In one long-term study tracking approximately 100,000 OSA patients, only 12% remained consistent CPAP users, highlighting the significant drop-off in adherence over time.
Mandibular advancement devices offer a less cumbersome alternative by repositioning the jaw to maintain an open airway. However, these devices can cause jaw discomfort, tooth movement, pain, or other complications. Surgical options, while effective for some, are invasive, expensive, and carry potential risks during both surgery and recovery.
The demand for non-invasive, patient-friendly alternatives has never been greater.
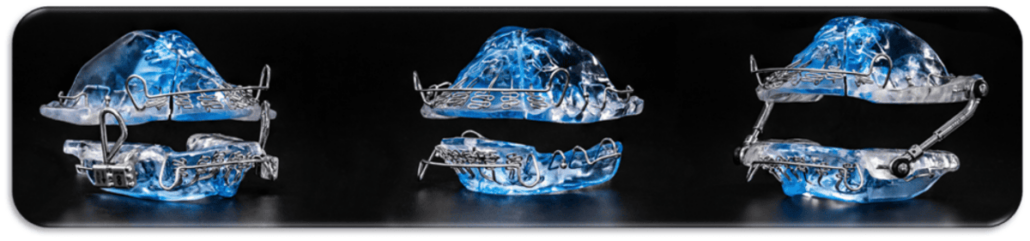
The Vivos CARE device: A paradigm shift
The Vivos CARE oral medical devices, powered by the proprietary Vivos Method, represent an innovative approach to treating obstructive sleep apnea (OSA) by addressing a primary root cause of the condition in many patients: craniofacial structural deficiencies. Unlike traditional therapies that manage symptoms, the CARE device targets the underdeveloped anatomy of the airway itself. Clinical data supports its effectiveness — results from 73 severe OSA patients submitted to the FDA showed that 97% of adult patients saw significant relief from OSA symptoms. Moreover, 80% experienced improvement of at least 50% reduction in the Apnea Hypopnea Index (AHI). The average treatment time was 9.7 months, after that no further interventions were required.
Think of it as non-surgical remodeling and rehabilitation of your airway. By leveraging the body’s natural capacity for bone remodeling, the CARE device promotes slow and sustained changes over 12 months or less. This process typically enhances airway size and stability, providing a long-term solution rather than a temporary fix. Patients often report noticeable improvements within weeks, including reduced symptoms, improved sleep quality, and greater energy levels during the day. Allen, a patient who used Vivos CARE devices, shared his experience: “Being only a short time into Vivos, it reduced the times I would fall asleep throughout the day, which included while I was driving. I have noticed a big difference. Not biting my tongue nearly as much, making eating more pleasant.”
This treatment is designed with patient preference and convenience in mind. Non-invasive and easy to use, it integrates seamlessly into nightly routines without the need for bulky machines, uncomfortable masks, or intrusive adjustments. This simplicity not only makes the therapy more appealing but also ensures higher compliance rates — a critical factor in successful OSA treatment.
This approach focuses on natural craniofacial development. By stimulating bone growth and expanding the airway, it addresses the structural issues underlying OSA, offering a treatment option that is effective, comfortable, and sustainable.
This patient-centered approach not only benefits individuals but also reduces the long-term strain on healthcare systems by minimizing complications associated with untreated OSA, such as cardiovascular disease and chronic fatigue. With its innovative design and clinical efficacy, the CARE devices mark a significant leap forward in how we approach OSA management, offering new hope for millions struggling with this pervasive condition.
Clinical implications of better sleep
Effective management of OSA delivers transformative benefits, not just for individual health outcomes but also for broader healthcare systems and societal well-being. Addressing OSA can significantly reduce the risk of cardiovascular conditions such as hypertension, arrhythmias, and stroke. Furthermore, studies demonstrate that treating OSA improves mental health by alleviating symptoms of anxiety and depression, enabling patients to lead more fulfilling, productive lives.
Beyond individual health, the societal benefits are substantial. Improved sleep leads to heightened workplace productivity, fewer fatigue-related errors, and decreased motor vehicle accidents, directly impacting economic and public safety metrics. Families of OSA patients also experience relief, as untreated sleep apnea often disrupts relationships due to irritability, fatigue, or partner disturbances caused by snoring.
For specific high-risk populations, the stakes are even greater. Research shows that 30–35% of heart failure patients suffer from OSA, making its treatment potentially life-saving. Addressing OSA in these patients has been linked to improved cardiac function, better oxygenation, and overall enhanced quality of life. Pediatric populations, too, see profound developmental benefits from early OSA intervention, as it prevents learning difficulties and behavioral challenges linked to sleep deprivation.
Ultimately, OSA treatment does more than improve sleep — it fosters comprehensive physical, mental, and social well-being.
Shifting the conversation around sleep health
Awareness remains a significant barrier to effective OSA treatment. Many medical providers and individuals either do not recognize the symptoms as part of a larger OSA diagnosis or dismiss them as minor inconveniences. For healthcare providers and device developers, this underscores the need for education and outreach to encourage earlier diagnosis and intervention.
Innovative therapies have the potential to revolutionize the management of OSA, particularly as these solutions gain international traction. Expanding access to cutting-edge treatments aligns with global health priorities and represents a critical step in addressing the widespread impact of sleep apnea.
Bridging gaps in treatment
As the healthcare industry continues to innovate, the focus must shift away from merely managing the disease state to finding and dispensing solutions that address the root cause and hold the potential for actually resolving the underlying problems. By exploring new technologies and advancing the dialogue on sleep health, hospital directors, IT specialists, and device manufacturers can play a pivotal role in transforming the future of OSA care.
For the millions living with this condition, these efforts represent more than just advancements in treatment — they offer a clear and current pathway to better sleep, improved health, and a renewed sense of well-being.
It’s essential to move away from the outdated paradigm of relying solely on CPAP as the primary treatment, which only manages the condition. Instead, we must embrace innovative solutions that aim to eliminate OSA altogether, offering a much more powerful and lasting impact.
About the author
Kirk Huntsman, Chairman and CEO, Co-Founder at Vivos Therapeutics, is a distinguished leader in the dental and healthcare industries, renowned for founding and growing successful dental service organizations (DSOs). In 1995, he founded Dental One, expanding it to over 165 practices across 15 states before its sale in 2008. He later led ReachOut Healthcare America, a Morgan Stanley Private Equity portfolio company, and established both Xenith Practices and Ortho Ventures. Since 2016, Kirk has served as CEO and chairman of Vivos, driving advancements in dental technology. As a founding member of the Association of Dental Support Organizations (ADSO), he continues to shape the industry’s future. For more about Vivos Therapeutics, visit: vivos.com