Rapid Profound Hypothermia (Suspended Animation) in Clinical Trials as a new approach to emergency care when CPR fails
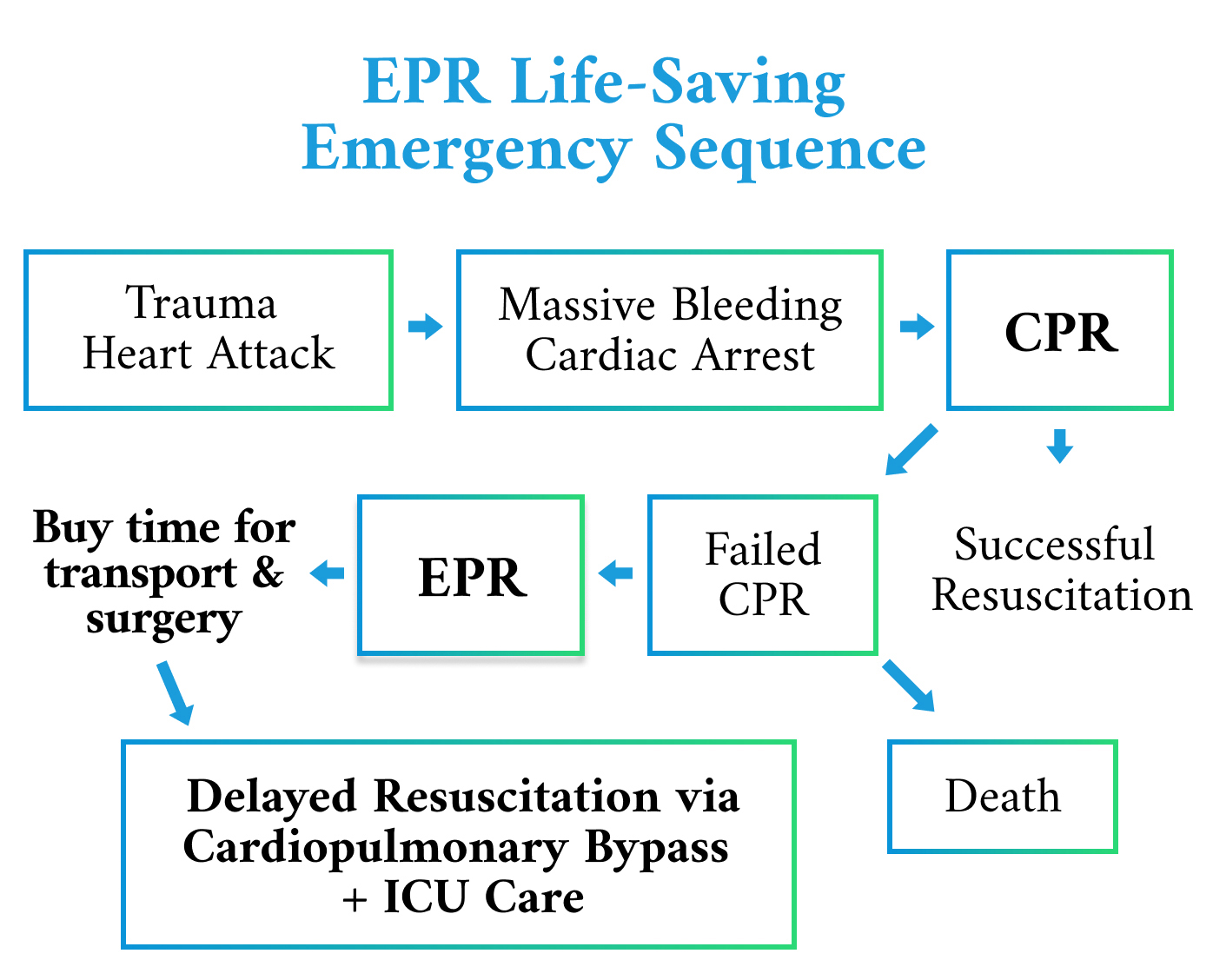
Emergency Preservation and Resuscitation (EPR), rapid profound hypothermia, is being pursued in clinical trials, as a revolutionary approach to be the next standard of emergency care to save lives when cardiopulmonary resuscitation (CPR) fails.
Approximately 2,000 people die each day in the U.S. from traumatic exsanguination (bleeding out) resulting from shootings, vehicular accidents, or other serious traumatic injuries, and from other causes of cardiac arrest despite receiving CPR. These numbers are alarming and cardiopulmonary resuscitation appears to be ineffective in most cases. To reduce this tragic loss of life, EPR-Technologies is pursuing development of an unprecedented standard of emergency care when CPR fails; namely, Emergency Preservation and Resuscitation. This innovative technology is geared towards providing hope for survival. The goal is to reduce the number of people who lose their lives during emergencies arising from shootings, sudden cardiac arrest, and vehicular accidents.
EPR-Technologies is a biomedical spinoff of the Safar Center for Resuscitation Research, University of Pittsburgh. Speaking on the launch of EPR-Technologies, the Chairman and CEO, Lyn Yaffe, M.D., said: “Rapid profound hypothermia has the potential to revolutionize resuscitation, providing one more chance to save a life when CPR fails, buying time for critical surgical and medical interventions, followed by delayed resuscitation and anticipated recovery. EPR hopes to set a new standard for emergency medical care. As always stated by Dr. Peter Safar, M.D., (1924-2003), the father of CPR and pioneer in rapid profound hypothermia, the goal is ‘to save hearts and brains too good to die.’ EPR-Technologies is dedicated to that goal.” The FDA-approved EPR feasibility clinical trial is being performed at Maryland Shock Trauma Center in Baltimore, MD. Initially, the technology was developed to help save the lives of fatally injured soldiers on the battlefield. The Army Medical Research and Materiel Command invested $17.5 million to date in cooperation with the Safar Center for Resuscitation to develop the Emergency Preservation and Resuscitation procedure.
Originally, EPR researchers used the term “suspended animation” to describe the impact of rapid profound hypothermia in their early experiments, a term very familiar in science fiction literature and movies. And like the current, preferable term “Emergency Preservation and Resuscitation”, suspended animation may be defined as treatment to preserve the viability of the entire organism during ischemia or lack of oxygen, such as during cardiac arrest. The goal of both the early experiments in suspended animation, and now also true for EPR, was to induce rapid profound hypothermia. Rapid profound hypothermia is a state in which no oxygen delivery is required for 3+ hours. This buys life-saving time for transport to a hospital followed by immediate surgical repairs and medical interventions, followed by restoration of the blood volume and delayed resuscitation, using cardiopulmonary bypass (CPB).
“Get cold enough, and you do OK with no blood for a while,” explained Samuel Tisherman, M.D., Professor of Shock Trauma Surgery, Maryland Shock Trauma, and Lead Trauma Surgeon for EPR. “We think we can buy time. We think it’s better than anything else we have at the moment and could have a significant impact on saving a bunch of patients. It’s called Emergency Preservation and Resuscitation (EPR). It’ll be a game-changer.”