New gene therapy appears to cure haemophilia
A Phase I/II multi-centre clinical trial, called B-AMAZE, has found that a single gene therapy injection dramatically reduces the bleeding risk faced by people living with haemophilia B and enabled trial participants to stop their regular blood clotting factor replacement therapy.
The study is published in the July 21, 2022 issue of the New England Journal of Medicine.
Of the 10 male patients selected to take part in the trial, all showed dose-dependent increases in factor IX levels. At a median follow-up of 27.2 months, sustained factor IX activity was observed in all the patients except one.
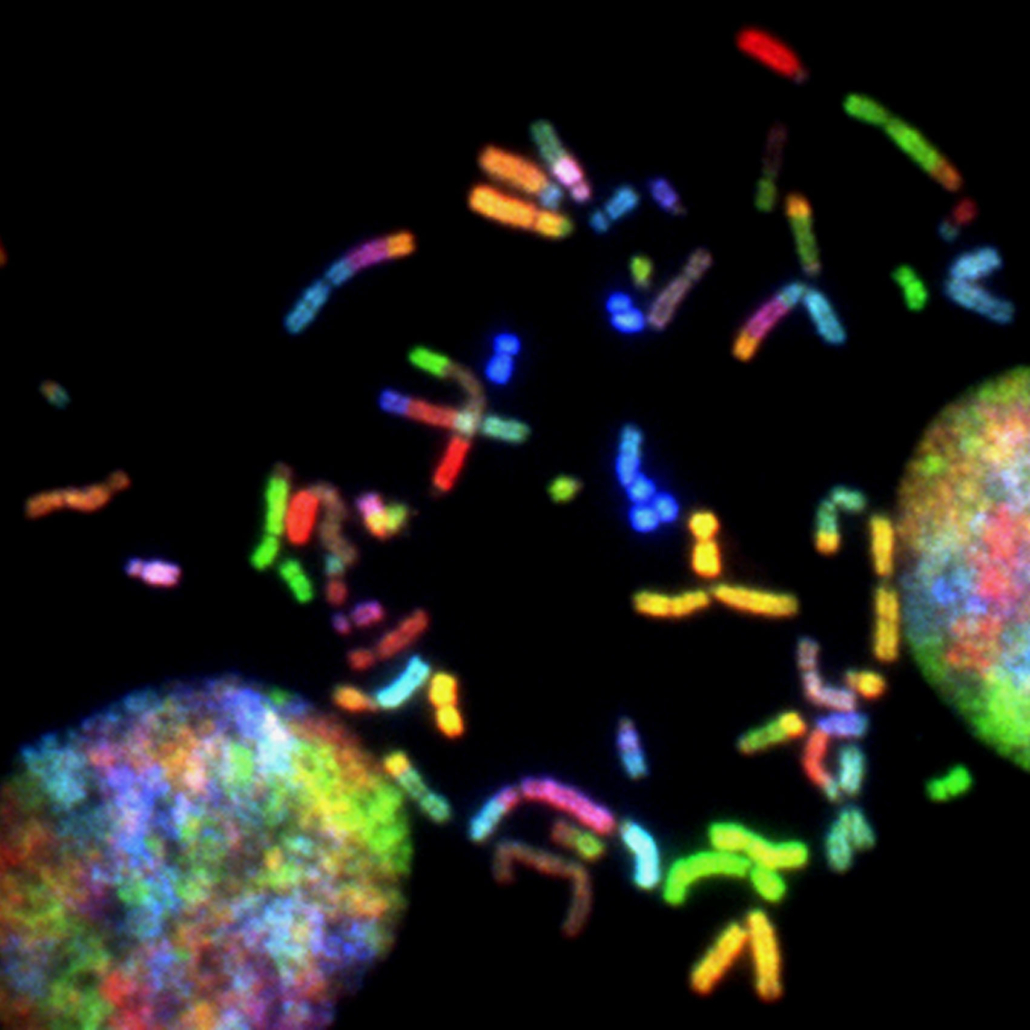
Haemophilia B is a rare and inherited genetic bleeding disorder caused by low levels of the blood clotting factor IX (FIX) protein.
The gene responsible for making FIX protein is located on the X chromosome, so the severe form of haemophilia B is much more common in men.
Currently, patients with haemophilia B need to inject themselves regularly – usually weekly – with recombinant FIX, a regular replacement therapy to prevent excessive bleeding. Despite advances in treatment, patients may continue to see debilitating joint damage.
The B-AMAZE trial and the related long-term follow up study found that one-time treatment with FLT180a led to sustained production of FIX protein from the liver in nine of ten patients, across four different dose levels. They no longer required weekly injections of FIX protein. They are also all enrolled in the long-term follow up study to assess safety and durability of FIX expression for 15 years.
FLT180a AAV gene therapy
FLT180a (verbrinacogene setparvovec) is a liver-directed adeno-associated virus (AAV) gene therapy. AAV gene therapy works by using a packaging from the proteins found in the outer membrane of the virus, to deliver a functional copy of a gene directly to patient tissues – in this case the liver. Newly synthesised proteins – in this case the FIX protein – are released into the blood. A one-time infusion can achieve long-lasting effects.
Lead author Professor Pratima Chowdary of the Royal Free Hospital, UCL Cancer Institute, said: “Removing the need for haemophilia patients to regularly inject themselves with the missing protein is an important step in improving their quality of life. The long term follow up study will monitor the patients for durability of expression and surveillance for late effects.”
Immunosuppression
Patients in the trial needed to take immune suppressing drugs over several weeks to several months, to prevent their immune systems from rejecting the therapy, and all reported known side effects. While the treatment was generally well tolerated, all patients experienced some form of adverse events, with an abnormal blood clot in one who received the highest FLT180a dose and had the highest levels of FIX protein.
Freeline Therapeutics co-founder Professor Amit Nathwani (UCL Medical Sciences), who co-authored the study, said: “Gene therapy is still a young field that pushes the boundaries of science for people with severe genetic diseases.
“The B-AMAZE long-term data add to the growing body of evidence that gene therapy has the potential to free patients from the challenges of having to adhere to lifelong therapy or could provide treatment where none exists today.”
Pamela Foulds, MD, Chief Medical Officer of Freeline, said: “The B-AMAZE long-term data continue to support our confidence that a single dose of FLT180a could protect people with haemophilia B from bleeding and the need for lifelong FIX replacement through durable expression of FIX at protective levels.”
The Phase I/II trial was sponsored by University College London and funded by Freeline Therapeutics, a clinical-stage biotechnology company developing AAV vector-mediated systemic gene therapies.
A Phase I/II dose-confirmation trial of FLT180a called B-LIEVE to finalize a dose for a Phase 3 pivotal trial is in progress.