Improving hygiene in endoscopy
The use of flexible endoscopes for endoscopic retrograde cholangiopancreatography (ERCP) is increasing as it represents a relatively non-invasive method for the diagnosis and treatment of certain conditions of the biliary and pancreatic ductal systems, such as gallstones, undefined biliary strictures, bile duct injury or leaks, and cancer. The design of duodenoscopes, however, is complex; they have long narrow channels and a recessed elevator at the distal end that enables good use of any accessories. All the external surfaces and internal channels are in contact with body fluids, presenting a risk of contamination and transmission of infection from patient to patient as well as from patient to endoscopy personnel. As these flexible devices are heat labile and not suitable for steam sterilization, careful cleaning (reprocessing) is needed to minimize the risk of contamination.
A recent event on Hygiene Solutions in Endoscopy was held at PENTAX Medical R&D Center (October 2019, Augsburg, Germany) to discuss insights on the need for infection control and how to minimize contamination. The event brought together a number of key opinion leaders in the field of ERCP hygiene (endoscopists, microbiologists and chief nurses) and included Paul Caesar, Hygiene and Infection Prevention expert at the Tjongerschans Hospital (Heerenveen, The Netherlands), Dr Hudson Garrett Jr., Global Chief Clinical Officer at PENTAX Medical and Assistant Professor of Medicine (Division of Infectious Diseases) at the University of Louisville School of Medicine, Kentucky, USA, as well as Wolfgang Mayer, Managing Director of Digital Endoscopy at PENTAX Medical.
Endoscopy-associated infection
The healthcare community is increasingly aware of the risk of hospital-acquired infection associated with endoscopy following documentation of several outbreaks of patient infections linked to duodenoscopes in the USA and around the world in the last decade as well as regulatory recalls. However, Paul Caesar made the point that in reality there is very little data regarding infection rates. One of the issues is that patients are discharged from hospital more and more quickly following procedures. Then, if any infection subsequently develops, the patient usually attends their local general practitioner and the link to the endoscopy is not made. The point was made that currently no surveillance is done for post-endoscopy infection and this should be put into place to generate reliable data on infection rates.
Endoscope reprocessing
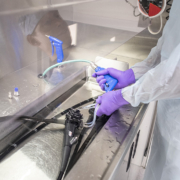
The role of endoscope reprocessing is crucial for mitigating the risk of infection and is achieved by mechanical cleaning detergent cleaning, high level disinfection, and rinsing and drying (Figs 1–3). However, research shows that in 45% of cases key reprocessing steps are skipped. Additionally, 75% of the reprocessing staff reported time pressures and non-compliance with guidelines related to reprocessing as a result. Paul Caesar emphasized this point saying, “Manual cleaning is still the most important step in reprocessing. However, in daily practice this stage is often downgraded to just a simple flush and brush. I call upon the field, to shift from reprocessing quantity to quality”. Another crucial step is to ensure that the device is thoroughly dried before storage. This reduces the risk of biofilm formation and bacterial growth. However, there are currently no official guidelines for the optimum drying time; even within Europe alone different countries use different drying times.
Suggestions for the improvement of reprocessing included:
1. proper explanation to and understanding by staff of the importance of the reprocessing stages to gain their commitment to following the procedure fully;
2. use of shorter visual pictogram explanations of the reprocessing stages rather than manuals that are approximately 150 pages long and are too complicated to thoroughly read and understand; and
3. traceability and tagging of the people performing the various tasks so that all the steps can be scanned and shown to be done in an optimal fashion.
Improving duodenoscope design
According to Calderwood et al., patient-to-patient transmission of infection has been linked to the elevator channel endoscopes (such as duodenoscopes) and attributed to persistent contamination of the elevator mechanism, the elevator cable and the cable channel. One solution to infection control is to use disposable duodenoscopes. However, this is not practical for every endoscopy because of the cost and the environmental impact. The one-time use of a disposable device is therefore recommended only for high-risk patients.
Hudson Garrett confirmed the company’s commitment to minimizing infection outbreaks with careful consideration of advice and requirements from the CDC (Centers for Disease Control and Prevention) and FDA (U.S. Food and Drug Administration) in the USA, and “using integrated feedback from all clinical stakeholders, optimizing reprocessing processes, and innovating products to directly tackle patient safety and infection prevention needs”. This has led to the development of a duodenoscope with a disposable distal cap with integrated elevator, hence eliminating the part of the device that is most associated with contamination. Additionally, use of the company’s dedicated dryer helps to ensure the device is fully dry, reducing the risk of microbial growth and subsequent potential contamination that can result from moisture. PENTAX Medical also has a strong commitment to the training of reprocessing staff, which (according to current data) requires a minimum of 8 hours to be done properly.