CAR T cells reduce atherosclerosis by 70% in mouse study
Scientists at the University of Pennsylvania’s Perelman School of Medicine have demonstrated that chimeric antigen receptor (CAR) T cell therapy could offer a novel approach to treating atherosclerosis.
Published in Circulation on 21 November 2025, the preclinical study shows engineered regulatory T cells reduced arterial plaque formation by approximately 70% in mouse models, marking the first application of CAR T technology to cardiovascular disease.
Engineering immune tolerance against oxidised LDL
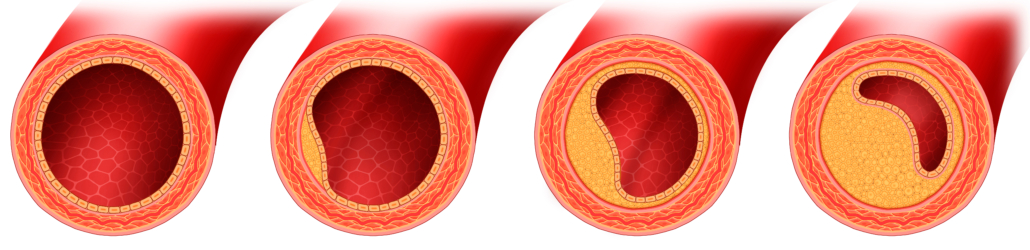
The research team engineered CAR regulatory T cells (CAR Tregs) to specifically target oxidised low-density lipoprotein (OxLDL), a key inflammatory driver in atherosclerotic plaque development. Unlike conventional CAR T therapies that activate immune responses against cancer cells, these modified Tregs dampen inflammation at sites of plaque formation.
“Our study shows for the first time how CAR T cell technology could be used to treat the underlying cause of the most common form of heart disease, which is the leading cause of death worldwide,” said senior author Dr Avery Posey, assistant professor of pharmacology at Penn Medicine.
The therapeutic approach addresses a critical gap in atherosclerosis treatment. Whilst statins effectively lower LDL cholesterol and lifestyle modifications reduce cardiovascular risk, no approved therapies specifically target the inflammatory pathways driving plaque progression.
Preclinical validation demonstrates mechanism of action
Initial in vitro experiments with human cells confirmed that anti-OxLDL CAR Tregs suppress inflammatory responses when exposed to oxidised LDL. The engineered cells significantly reduced foam cell formation, a hallmark of atherosclerotic plaques that occurs when macrophages accumulate cholesterol-laden lipid droplets.
The authors note in their paper: “Anti-OxLDL CAR Tregs mitigate inflammation and plaque deposition associated with oxidised LDL and may offer a new therapeutic option for atherosclerosis.”
The researchers then developed a murine version of the therapy and tested it in genetically engineered mice predisposed to hyperlipidaemia and atherosclerosis. These immunocompetent mouse models, which express human apolipoprotein B at physiological levels, closely replicate human lipoprotein metabolism and plaque formation.
After approximately 12 weeks of treatment, mice receiving anti-OxLDL CAR Tregs exhibited a mean plaque burden of 3.19% compared to 13.03% in control animals—representing roughly 70% reduction. Histological analysis revealed not only decreased plaque size but also increased collagen content surrounding arterial plaques, suggesting enhanced plaque stability and reduced rupture risk.
Immunosuppression without systemic toxicity
A significant finding was the absence of systemic immune dysfunction in treated animals. Flow cytometry analysis showed the engineered Tregs accumulated in both lymphoid tissue and atherosclerotic lesions, with elevated expression of transforming growth factor beta (TGFβ).
Lead author Dr Robert Schwab, instructor of haematology-oncology at Penn Medicine, explained: “OxLDL is a pro-inflammatory molecule, and that inflammation is what starts atherosclerosis. The idea was, if we can get the immune system to see OxLDL and provoke an anti-inflammatory response, it would reduce inflammation and essentially stop the pathogenesis in its tracks.”
Mechanistic studies revealed that TGFβ secreted by activated CAR Tregs mediated the reduction in macrophage lipid uptake and promoted polarisation towards an anti-inflammatory M2-like phenotype. This effect was abolished when anti-TGFβ antibodies were added to co-cultures, confirming TGFβ’s essential role in the therapeutic mechanism.
Importantly, serum cytokine profiling throughout the treatment period showed no sustained inflammatory responses, and lipid levels remained unchanged between treatment groups. These findings suggest the immunomodulatory effects were localised to the vascular microenvironment rather than producing systemic immunosuppression.
Addressing residual cardiovascular risk
Co-author Dr Daniel Rader, chair of genetics at Penn Medicine, emphasised the clinical relevance: “The idea that therapy targeted to inflammation within the arterial wall can reduce the risk of atherosclerotic cardiovascular disease is compelling. The use of a CAR T approach to target the proinflammatory molecule oxLDL could provide an important complementary treatment approach to reducing the high residual risk of atherosclerotic cardiovascular disease in patients on effective cholesterol-lowering therapy.”
The research has particular significance for cancer survivors, who face elevated cardiovascular risk from both treatment-related cardiotoxicity and cancer-associated inflammation. Dr Schwab noted: “Cancer, inflammation, and heart disease go hand-in-hand. It’s a real shame to see a patient cured of cancer die from a heart attack a year or two later.”
Translation pathway and next steps
The researchers and Penn Medicine have founded Cartio Therapeutics to advance the OxLDL CAR Treg therapy towards clinical trials. However, several questions remain before human testing can proceed.
The current study documented prevention of plaque formation rather than regression of established lesions, as treatment began concurrently with hyperlipidaemia induction. Whether CAR Tregs can reverse existing atherosclerotic disease requires further investigation.
Additionally, differences in CAR T cell biology between mice and humans, particularly regarding persistence and functional longevity, necessitate validation in humanised models that better recapitulate human atherosclerosis. The authors acknowledge these limitations whilst noting that their syngeneic immunocompetent mouse models avoid the confounding effects of immunodeficiency.
The research received funding from the Hematology Research Training Program, the American Society of Hematology Research Training Award for Fellows, and the Department of Veterans Affairs.
Reference
Schwab, R.D., Degaramo, D., Hong, S.J., et. al. (2025). OxLDL-targeted chimeric antigen receptor T regulatory cells reduce atherosclerotic plaque development. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.125.073987