Advanced ultrasonic protein removal technology: set to change how surgical instruments are cleaned
Standard methods of decontamination, such as Disinfector Washers (e.g. using hot alkaline solutions and surfactants), are known to be inconsistently effective in removing protein from surgical instruments. Advanced Ultrasonics offers an exciting and tantalizing alternative. Preliminary results suggest that intense cleaning using “advanced ultrasonic technology” can potentially result in disinfection without the need for any thermal or chemical methods.
by David Jones
In the UK, concerns about Creutzfeldt-Jacob Disease (CJD) date back to the mid-1980s when an outbreak of Bovine Spongiform Encephalopathy (BSE, a similar transmissible neuro-degenerative brain disease) in cattle raised concerns that the disease might be transmissible to humans. Confirmation came in 1996 [1] that BSE can indeed lead to a form of human CJD (variant (v)CJD) that particularly affected younger adults. This resulted in widespread public health concern, heightened again a few years ago when a study in the British Medical Journal [2] suggested that as many as 1 in 2000 Britons may be infected with the abnormal prion protein that causes vCJD. To date there have been 178 deaths due to vCJD in the UK with a few more elsewhere [3]. In both model experiments and in actual human studies it has been shown that the prion protein is readily transmitted on stainless steel instruments from one animal to another.
vCJD highlighted to clinicians and decontamination / sterile services professionals alike, the critical requirement to remove protein, as well as other infectious agents, from neuro-surgical and other reusable surgical instruments. In addition to the risk of patient-to-patient transferal of vCJD prions, there is a danger that bacteria hidden in or under any residual protein e.g. biofilms could also be passed on. A recent study in the journal Acta Neuropathologica [4] also highlighted the potential dangers associated with cross-contamination of neurosurgical instruments with the peptide amyloid beta (Aβ), a substance implicated in brain hemorrhages and Alzheimer’s disease.
Standard methods such as Disinfector Washers (e.g. hot alkaline solutions and surfactants) are known to be inconsistently effective in removing protein from surgical instruments [5,6] and other difficulties in ensuring consistent cleanliness has led to a move towards single use instruments. However, questions remain as to how manufacturers of single use instruments can achieve consistent cleanliness and sterility when modern, well equipped Sterile Service and Decontamination (SSD) units apparently cannot. Unfortunately, single use instruments are not always clean and sterile as recent unpublished investigations have shown.
In the UK, concerns about contamination mean that GPs and dentists, who have historically performed minor interventions such as lancing of boils, removal of small cysts and abscesses etc., are now being discouraged from doing so. This, in turn, is funnelling more patients to A&E departments, which are already under tremendous strain. Post-operative infections also add to strain on the health service, leading to extended hospital stays and bed-blocking.
There is a clear need for a new approach to improve the cleaning of surgical devices. “Commercial grade” ultrasonic cleaning systems have been available for a number of years and have been used as a first stage in the cleaning process.
Ultrasonics works via the process of cavitation. Transducers bonded to the base or side of a tank are excited by high frequency electricity causing them to expand and contract at very high speed. This mechanical action causes high speed downward flexure of the radiating tank face. The speed of this movement is too fast for the water in the tank to follow, resulting in the production of vacuum chambers. On the upward flexure the vacuums are released in the form of vacuum bubbles which rise up through the fluid until they hit an object, upon which the bubbles implode under high pressure, thus drawing away any contamination that may be on the surface of the object.
However, it has been shown that machines used in sterile services departments in the past have an erratic distribution of sound that does not consistently render instruments clear of residual protein. It was felt by many that a new way of applying ultrasound into a fluid was required. To achieve the safe cleaning of these items, the sound needs to be applied in a way that is both even as well as intense, with no gaps in activity where cleaning would not be effective.
In order to develop a new cleaning technology, a reliable method for measuring residual protein was needed and agreement reached on acceptable levels. The UK HTM 01-01 Guidance on the Management and Decontamination of Surgical Instruments [7], released in 2016, specifies that “there should be <5µg of protein in situ, on a side of any instrument tested”. In situ testing is specified since: “detection of proteins on the surface of an instrument gives a more appropriate indication of cleaning efficacy related to prion risk” than the swabbing techniques used in the past [8,9,10]. Currently the ProReveal system, from Synoptics Health, Cambridge UK, is the only in situ system on the market worldwide. As well as high levels of accuracy, the system also identifies the precise location of any remaining proteins on the instrument. To comply with UK HTM 01-01 guidance, therefore, any new cleaning system, ultrasonic or otherwise, needs to be validated against the levels of detection offered by ProReveal.
A second issue to be addressed by any ultrasonic cleaning technology is how to measure the ultrasonic activity. HTM 01-01 states that machines should be periodically tested for ultrasonic activity.
Historically, the only method available to Sterile Services Managers and AED’s for validating the activity in an ultrasonic tank has been to insert a piece of aluminium foil into the fluid for a set time and then visually analyse the indentations in the foil to determine the ultrasonic activity. This is a somewhat inaccurate way of validating what is a critical phase in the decontamination process. Troughs of sound can be either macroscopic or microscopic and, as such, the reliance on sight alone is unacceptable when such high levels of consistent cleanliness are expected.
With both these issues in mind, Alphasonics (a Liverpool/UK company with over 25 years’ experience in the field of ultrasonic cleaning systems) launched the ‘Medstar’ project with a view to developing ‘advanced ultrasonic technology’ for cleaning surgical equipment. The project started in 2013 but it was not until 2015 when a ProReveal was purchased that substantive advances were made. Progress then accelerated quickly and over a 3-year period, a point was reached whereby instruments could be rendered “completely” free of residual protein, as assessed by ProReveal technology.
To overcome the problems around accurately measuring ultrasonic activity, the world’s first Cavitation Validation Device (CVD) was developed from 2016 to 2018 which, for the first time, allows the validation of ultrasonic cleaning devices by listening exclusively for cavitation noise.
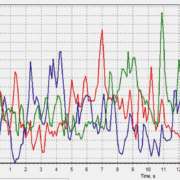
CVDs are included within most Medstar systems and the below graphs show how Medstar devices perform compared to existing ‘commercial grade’ ultrasonic cleaners (Data on File).
It is this unique, intense ultrasound technology that is so effective in removing protein residue from medical devices, as measured by the in situ ProReveal method. To assess the effect on removal of bacteria, a UKAS (UK Accreditation Service) accredited laboratory was engaged to carry out independent trials. Instruments were contaminated by the laboratory, first with Enterococcus faecium and Staphlyococcus aureus (as specified within ISO15883 annex N- “test soils and methods for demonstrating cleaning efficacy”) and then with “dirty” conditions (specified in ISO13727). They were then cleaned in a Medstar device. Since all residual protein was being removed, the question arose: was the (now exposed) bacteria also being removed by the intense ultrasound?
Work is on-going, but preliminary results suggest that intense cleaning using ‘advanced ultrasonic technology’ can potentially result in disinfection without the need for any thermal or chemical methods.
Medstar devices have several other features to allow compliance with UK HTM01-01 guidance, such as the Generator Output Monitoring System- which constantly monitors the generator output and adjusts the input accordingly, thus ensuring that the system is always performing optimally. The CVD device is then used for periodic independent validation.
Advanced Ultrasonics offers an exciting and tantalizing alternative to thermal disinfection devices. The HTM01-01 UK guidelines are only the start of things to come and it is already widely recognized that the 5µg limit set out in the guideline is still too high. The many trials undertaken by the manufacturer have clearly shown that the Medstar range of equipment leaves no more than 0.5µg of residual protein per side on an instrument and as such renders the bacteria fully exposed to the intense, very even, action of the ultrasound and enzymatic chemicals.
High throughput systems are also available that would be of great benefit to single-use instrument manufacturers and SSD units alike. These systems will deliver a consistently lower residual protein count and a better log reduction than thermal disinfection devices.
References
1. John Collinge, Katie CL Sidle, Julie Meads, James Ironside, Andrew F Hill. Molecular analysis of prion strain variation and the aetiology of “new variant” CJD. Nature, 1996; 383(6602), 685. doi:10.1038/383685a0
2. Gill O, Spencer Y, Richard-Loendt A, Kelly C, Dabaghian R, Boyes L, Linehan J, et al. Prevalent abnormal prion protein in human appendixes after bovine spongiform encephalopathy epizootic: large scale survey. British Medical Journal, 2013; 347, 11.
3. See www.cjd.ed.ac.uk/sites/default/files/figs.pdf
4. Jaunmuktane Z, Quaegebeur A, Taipa R, Viana-Baptista M, Barbosa R, Koriath C, Sciot R, et al. Evidence of amyloid-β cerebral amyloid angiopathy transmission through neurosurgery. Acta Neuropathologica, 2018; 135(5), 671–679. doi:10.1007/s00401-018-1822-2
5. Murdoch H, Taylor D, Dickinson J, Walker JT, Perrett D, Raven NDH, Sutton JM.
Surface de-contamination of surgical instruments – an ongoing dilemma. Journal of Hospital Infection 2016; 63: 432-438
6. Baxter RL, Baxter HC, Campbell GA, Grant K, Jones A, Richardson P, Whittaker G. Quantitative analysis of residual protein contamination on reprocessed surgical instruments. J Hosp Infect 2006; 63, 439-444.
7. Department of Health and Social Care. Health Technical Memorandum (HTM) 2006; 01-01: management and decontamination of surgical instruments (medical devices) used in acute care.. Available: https://www.gov.uk/government/publications/management-and-decontamination-of-surgical-instruments-used-in-acute-care. Last accessed July 2018.
8. Nayuni N, Cloutman-Green E, Hollis M, Hartley J, Martin S, Perrett D. A critical evaluation of ninhydrin as a protein detection method for monitoring surgical instrument decontamination in hospitals. J Hospital Infection 2013; 84 97-102
9. Nayuni N, Perrett D. A comparative study of methods for detecting residual protein on surgical instruments. Medical Device Decontamination (incorporating the IDSc Journal) 2013; 18 16-20
10. Perrett D, Nayuni N. Efficacy of current and novel cleaning technologies (ProReveal) for assessing protein contamination on surgical instruments 2014; Chapter 22 in Decontamination in Hospitals and Healthcare Edited by Dr. J.T. Walker, Woodhead Publishers, Cambridge, UK.
The author
David Jones
Alphasonics, Liverpool, UK
www.alphasonics.co.uk