Eye implant restores reading vision in geographic atrophy patients
A wireless subretinal photovoltaic implant paired with augmented-reality glasses has enabled patients with complete central vision loss from geographic atrophy to read letters, numbers and words, according to results from a European clinical trial published in The New England Journal of Medicine on 20 October 2025.
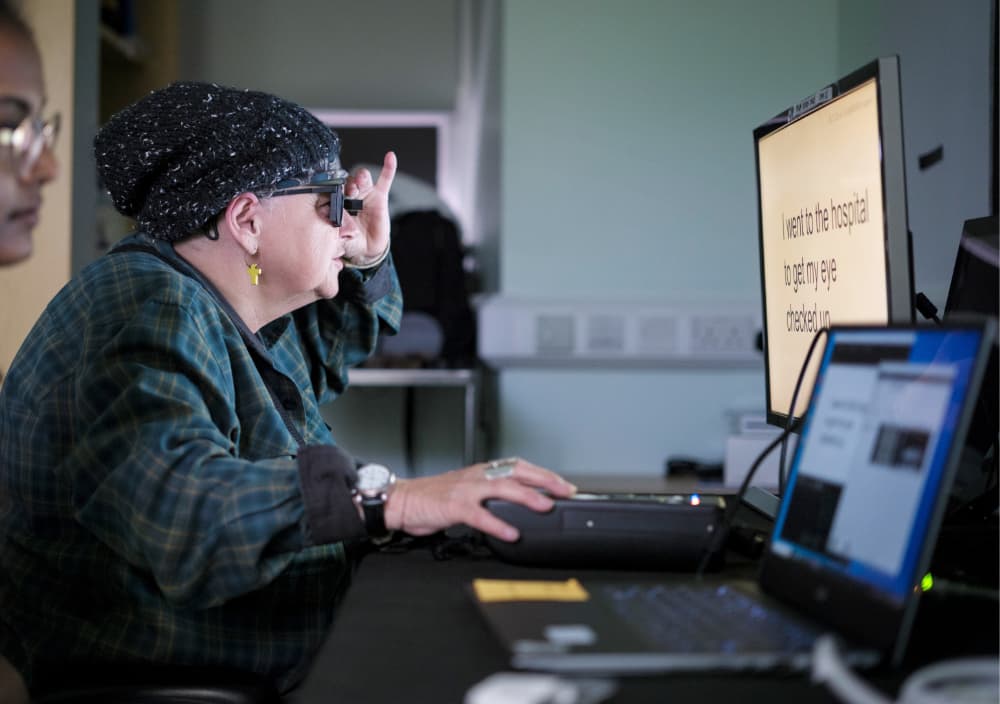
Study partipant Sheila Irvine, a patient at Moorfields, training with the PRIMA device © Moorfields Eye Hospital
Clinical trial demonstrates vision restoration in untreatable condition
The multicentre trial involving 38 patients across 17 hospital sites in five countries tested the PRIMA device, marking the first time an artificial vision system has successfully restored reading ability through eyes that had lost their sight. Eighty-four per cent of participants achieved the ability to read using prosthetic vision, with patients reading an average of five lines on a vision chart where many could not previously see the chart at all.
All participants had lost complete central sight from geographic atrophy with dry age-related macular degeneration (AMD), a condition affecting 5 million people globally for which no treatment currently exists. Geographic atrophy involves progressive deterioration of macular cells, with light-sensitive retinal cells dying off and the central macula degenerating, leaving only limited peripheral vision.
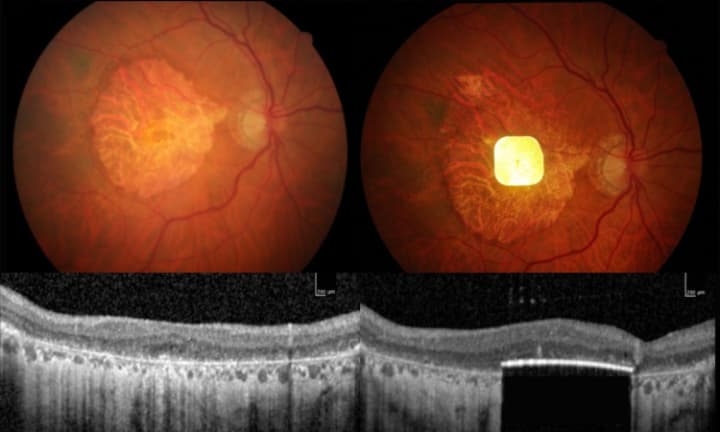
Image of the chip in a patient’s eye © Science Corporation
Surgical implantation and activation process
The procedure involves a standard vitrectomy followed by insertion of an ultra-thin microchip measuring 2mm × 2mm and 30 micrometres thick, approximately half the thickness of a human hair. Surgeons create a trapdoor beneath the centre of the patient’s retina to position the chip in the subretinal layer, under the deceased retinal cells.
Mahi Muqit, associate professor in the UCL Institute of Ophthalmology and senior vitreoretinal consultant at Moorfields Eye Hospital, who led the UK arm of the trial, said: “In the history of artificial vision, this represents a new era. Blind patients are actually able to have meaningful central vision restoration, which has never been done before.”
The operation can be performed by trained vitreoretinal surgeons in under two hours. Approximately one month post-surgery, once the eye has stabilised, the chip is activated through augmented-reality glasses containing a video camera connected to a small waistband computer with zoom functionality.
Technical mechanism and rehabilitation
The video camera projects the visual scene as an infrared beam directly across the subretinal chip, functioning as a miniature solar panel. Artificial intelligence algorithms process this information through the pocket computer, converting it into electrical signals that pass through retinal and optic nerve cells to the brain for interpretation as vision.
Patients undergo intensive rehabilitation programmes spanning several months to learn signal interpretation and restore reading ability. The training enables them to focus and scan across objects in the projected image, using the zoom feature to enlarge text. Trial participants were encouraged to explore additional applications beyond reading, with some using the device for puzzle-solving and metro navigation.
Safety profile and future applications
No significant decline in existing peripheral vision was observed in trial participants, an important safety consideration for the surgical approach. The findings establish the foundation for seeking regulatory approval to market the device.
Sheila Irvine, a Moorfields patient on the trial, said: “I was an avid bookworm, and I wanted that back. It’s not simple, learning to read again, but the more hours I put in, the more I pick up. Reading takes you into another world, I’m definitely more optimistic now.”
Muqit noted potential broader applications: “I think it’s something that, in future, could be used to treat multiple eye conditions.” He emphasised that rehabilitation remains crucial, stating: “It’s not like you’re popping a chip in the eye and then you can see again. You need to learn to use this type of vision.”
The global trial was led by Dr Frank Holz of the University of Bonn, with Moorfields Eye Hospital serving as the sole UK site. The PRIMA System device is being developed by Science Corporation (science.xyz), which specialises in brain-computer interfaces and neural engineering.
Reference
Holz, F. G., et al. (2025). Vision restoration with a neurostimulation system in geographic atrophy due to AMD. New England Journal of Medicine. https://doi.org/10.1056/NEJMoa2501396

