Novel Human Skin Atlas reveals developmental secrets and potential for regenerative medicine
A groundbreaking study has mapped prenatal human skin at the cellular level, offering unprecedented insights into skin formation and hair follicle development. The research, which includes the creation of a novel skin organoid model, could pave the way for developments in treating congenital skin disorders and improving regenerative medicine approaches.
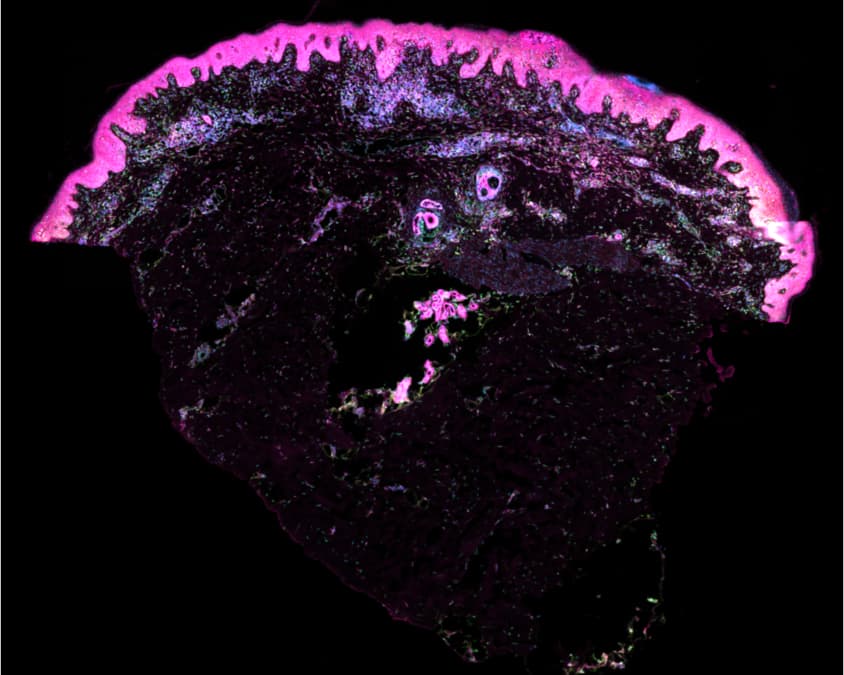
Cell segmentation stain of human skin using the xenium cell segmentation antibody panel.
Pink = cell membrane
Blue = nuclei
Yellow/Green = internal cell stain
© Wellcome Sanger Institute
Researchers from the Wellcome Sanger Institute and Newcastle University have created the first single-cell atlas of prenatal human skin, providing a detailed molecular ‘recipe’ for skin formation. The study, published in Nature on 16 October 2024 [1], utilised cutting-edge genomic techniques to analyse individual cells in space and time, uncovering the intricate processes that regulate skin and hair follicle development.
The team employed single-cell sequencing and spatial transcriptomics to examine prenatal skin tissue samples, allowing them to track cellular changes throughout development. This approach revealed key differences between human and mouse hair follicle formation, highlighting the importance of human-specific models in dermatological research.
Dr Elena Winheim, co-first author from the Wellcome Sanger Institute, explained: “With our prenatal human skin atlas, we’ve provided the first molecular ‘recipe’ for making human skin and uncovered how human hair follicles are formed before birth. These insights have amazing clinical potential and could be used in regenerative medicine, when offering skin and hair transplants, such as for burn victims or those with scarring alopecia.”
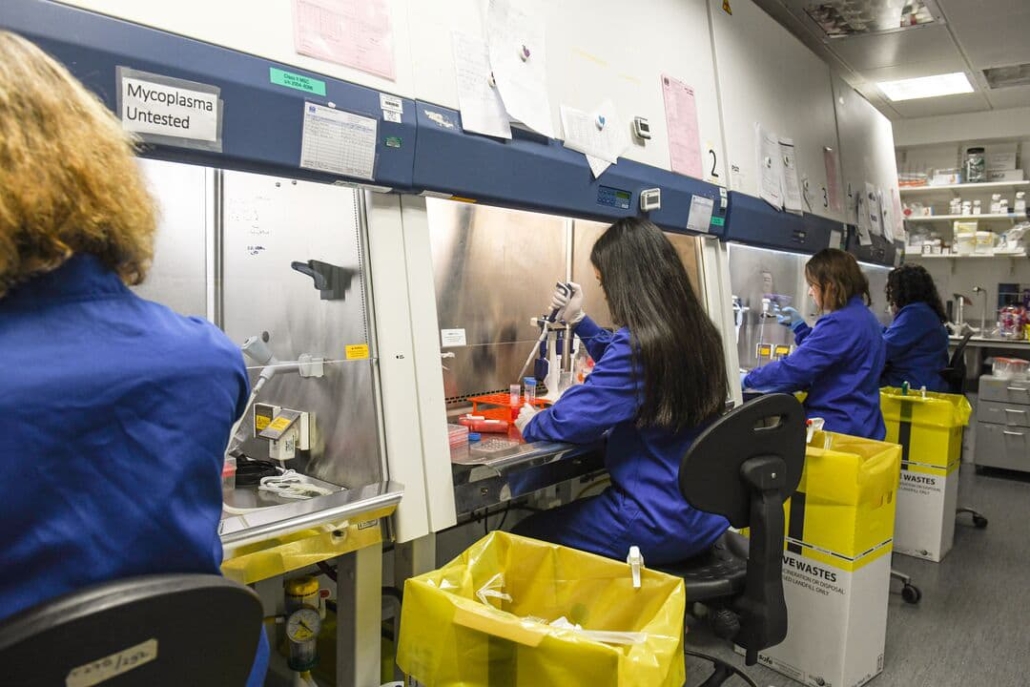
Changing growth media on skin organoids, laboratory work at the Wellcome Sanger Institute.
© Greg Moss / Wellcome Sanger Institute
The role of immune cells in skin development
One of the study’s most significant findings was the discovery of a previously unknown role for macrophages in prenatal skin development. These immune cells were found to promote blood vessel formation in developing skin tissue, a process crucial for proper skin function.
Dr Hudaa Gopee, co-first author from Newcastle University, noted: “We’re excited to have made a skin organoid model that grows hair. In this process, we uncovered a new, important role of immune cells in promoting the growth of blood vessels in developing skin tissue, which could help improve other organoid models.”
The researchers also observed that macrophages appear to play a key role in the scarless healing ability of prenatal skin. This finding could have significant implications for developing new approaches to prevent scarring after surgery or injury in adults.
Creating a ‘mini organ’ of skin
In addition to mapping prenatal skin development, the team successfully created a skin organoid capable of growing hair. This ‘mini organ’ closely resembled prenatal skin in its molecular characteristics, offering a valuable new model for studying congenital skin diseases and testing potential treatments.
The organoid model also provided insights into the limitations of current tissue engineering approaches. By identifying the absence of blood vessels in the initial organoid, the researchers were able to improve the model by adding macrophages, which promoted vascularisation.
Implications for congenital skin disorders
The prenatal human skin atlas offers new opportunities for understanding the origins of congenital hair and skin disorders. The researchers found that genes associated with conditions such as blistering disorders and scaly skin are expressed in prenatal skin, indicating that these conditions originate in utero.
This knowledge, combined with the newly developed skin organoid model, provides researchers with powerful tools for investigating the mechanisms underlying these disorders and developing targeted therapies.
Advancing regenerative medicine
The molecular ‘recipe’ for skin formation uncovered in this study has significant potential for regenerative medicine applications. The insights gained could be used to improve techniques for creating new hair follicles and enhancing skin grafts for burn victims or individuals with extensive scarring.
Professor Muzlifah Haniffa, co-lead author and Interim Head of Cellular Genetics at the Wellcome Sanger Institute, emphasised the broader implications of the research: “Our prenatal human skin atlas and organoid model provide the research community with freely available tools to study congenital skin diseases and explore regenerative medicine possibilities. We are making exciting strides towards creating the Human Cell Atlas, understanding the biological steps of how humans are built, and investigating what goes wrong in disease.”
Human Cell Atlas initiative
As part of the Human Cell Atlas initiative [2], which aims to map all cell types in the human body, this research represents a significant step forward in understanding human development and disease. The freely available data from the human skin atlas [3] can be explored through an interactive web portal, facilitating further research and collaboration in the field.
Reference:
- Gopee, N. H., Winheim, E., et al. (2024). A human prenatal skin cell atlas reveals immune cell regulation of skin morphogenesis. Nature. https://doi.org/10.1038/s41586-024-08002-x
- https://www.humancellatlas.org
- https://developmental.cellatlas.io/fetal-skin

